In this ACLS Megacode scenario, use the appropriate ACLS algorithms to treat the patient. There are 17 questions for this ACLS megacode scenario.
Quiz Summary
0 of 17 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 17 Questions answered correctly
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 17
1. Question
Scenario data: A 65-year-old male collapses as he is out for his morning walk. A bystander witnessed the collapse, activates EMS, and begins CPR. The EMS team arrives 6 minutes later. The monitor is attached and the assessment is as follows:
Skin: cold/clammy/cyanotic
Cardiovascular: no pulse
Respiratory: no respirations
CNS: no response
Monitor: rhythm strip below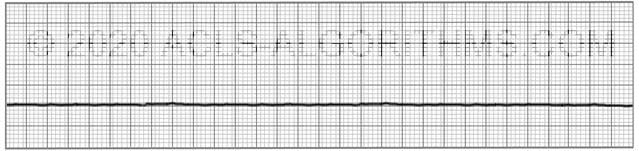
What ACLS algorithm are you going to begin this scenario with?
CorrectIncorrect -
Question 2 of 17
2. Question
As an EMS provider in the out of hospital setting, your first step is to:
CorrectIncorrect -
Question 3 of 17
3. Question
While the EMS team is providing 5 cycles of CPR what other activities can be completed?
CorrectIncorrect -
Question 4 of 17
4. Question
After your IV is secure, your next step involves giving a medication. What medication should be used?
CorrectIncorrect -
Question 5 of 17
5. Question
(True or False)
Vasopressin 40 U IV can replace the 1st or 2nd dose of epinephrine in the cardiac arrest algorithm.CorrectIncorrect -
Question 6 of 17
6. Question
Epinephrine should be repeated at what frequency for the treatment of Asystole?
CorrectIncorrect -
Question 7 of 17
7. Question
You give epinephrine 1 mg IV and finish the cycle of CPR. What is your next intervention?
CorrectIncorrect -
Question 8 of 17
8. Question
After giving the first dose of epinephrine you finish the cycle of CPR. A rhythm check shows that the patient's rhythm changed from asystole to the rhythm below. He also remains pulseless. Your first action is to:
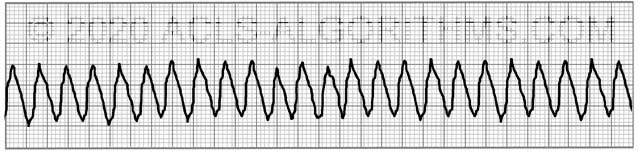 CorrectIncorrect
CorrectIncorrect -
Question 9 of 17
9. Question
You deliver 1 shock of 120J. After the shock what is the your next step?
CorrectIncorrect -
Question 10 of 17
10. Question
You have resumed CPR. Your next intervention after 5 cycles of CPR is to:
CorrectIncorrect -
Question 11 of 17
11. Question
Your rhythm check reveals continued pulseless VT. What are your next 2 steps?
CorrectIncorrect -
Question 12 of 17
12. Question
You give a second shock and perform 5 cycles of CPR. What medication should you give after the second shock during CPR?
CorrectIncorrect -
Question 13 of 17
13. Question
The epinephrine is given and the round of CPR completed. A rhythm check reveals no change in the rhythm and pulseless VT continues. You shock with 300 J and start another cycle of CPR. What medication are you going to give at this time?
CorrectIncorrect -
Question 14 of 17
14. Question
You give amiodarone 300 mg IV and finish the cycle of CPR, your rhythm check reveals continued pulseless VT, continuing on, you shock the patient with 360 J. What is your intervention at this time.
CorrectIncorrect -
Question 15 of 17
15. Question
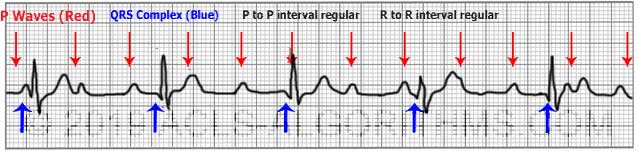
After completing 5 cycles of CPR a rhythm check reveals the following:

Your pulse check reveals a faint palpable pulse. VS are: HR 30; BP 78/58; and the patient does not have spontaneous breathing. What is the next step?
CorrectIncorrect -
Question 16 of 17
16. Question
You recognize this rhythm because there is no apparent relationship between the P-waves and the QRS complexes. What is the rhythm?
 CorrectIncorrect
CorrectIncorrect -
Question 17 of 17
17. Question
After you initiate TCP the patient continues to stabilize. VS are: HR 70; BP 105/75; RR 5; You continue to support ventilation with the bag valve mask, and TCP continues. If transcutaneous pacing was not available, what medication can be considered as an alternative?
CorrectIncorrect
Cecilia says
Your site is so thorough, love it. THANK U. Thank you also for responding to our questions. Q15. The strip looks to me like HR is about 50, 3rd deg HB. But you say 30, faint pulse. Can you help me interpret strip?
Jeff with admin. says
You are correct, the strip is 3rd degree block. The ventricular rate is 50/min on the monitor and the atrial rate is 120/min. The pulse by palpation is 30/min. Directly post arrest, there can be a discrepancy between the rate by palpation and the electrical rate. 3rd degree block can make this even worse because of the poor perfusion related to the 3rd degree block.
Kind regards,
Jeff
mjbaker779 says
Atropine is before TCP in the Brady algorithm.
Jeff with admin. says
You could attempt Atropine 0.5mg IV push however, since this patient has been unstable and the defibrillator/pacer is already attached to the patient, TCP, should not be delayed. If for some reason TCP could not be initiated immediately, you could attempt atropine 0.5mg IV push.
Kind regards, Jeff
Robel says
Isn’t securing the airway part of the CPR? Would one be able to deliver breathes without securing the airway? I thought we would proceed to the next step like establishing an IV.
Jeff with admin. says
Yes securing the airway is part of CPR. However, securing the airway means that you are using some type of device to ensure that the airway remains open. This would be with something like an oropharyngeal airway (OPA), laryngeal tube device, or intubation. Head tilt chin lift would not be considered securing the airway. That would be opening the airway. I’m not sure which question you were asking about so I had to give my best guess at which one you were referring to.
Kind regards,
Jeff
Connie Rummel says
In qustion 15, after a return of a pulse, since this person is not breathing, wouldn’t the priority be to address oxygenation before transcutaneous pacing? Wouldn’t one team member want to continue rescue breathing while another team member starts transcutaneous pacing?
Jeff with admin. says
Rescue breathing would be an important intervention, but it was not included as one of the multiple choice questions. Since the defibrillator is attached and the patient has poor perfusion (HR of 30 and the BP of 78/58), the best answer would be to initiate TCP (transcutaneous pacing). TCP would support the circulation and most likely improve perfusion.
Kind regards,
Jeff
sarahgudger says
On question #15, if it were “Atropine 0.5mg,” would this be the next step I should follow before TCP?
Thanks.
Jeff with admin. says
You could attempt Atropine 0.5mg IV push however, since this patient has been unstable and the defibrillator/pacer is already attached to the patient, TCP, should not be delayed. If for some reason TCP could not be initiated immediately, you could attempt atropine 0.5mg IV push. Kind regards, Jeff
fourleafclover6 says
Isn’t Atropine contraindicated in high degree blocks? It won’t work!
Also on Question #11->You give a second shock and perform 5 cycles of CPR. What medication should you give after the second shock during CPR? Answer was Epi, why is it not Amiodarone? 1 round of Epi has been given, 2 refractory shocks, is it Epi Because it has been 3-5 min? I thought it was Amio because Epi had been given and the PT remained in Cardiac Arrest (VT) refractory to CPR, EPI and Shock; can you please clarify?
Jeff with admin. says
Question 1: Atropine would probably not work. However, it would not be contraindicated. It won’t hurt anything. It just would not work.
Question: 2: Technically, When you switch from the right branch of the Cardiac Arrest Algorithm (PEA/Asystole), you would start at the top of the algorithm. In this case, starting at the top of the algorithm, epinephrine would be given after the 2nd shock and then amiodarone would be give after the 3rd shock. There are many who would do as you said and consider the earlier dose of epinephrine as the first dose given. There is debate about this, but it would be slightly diverging away from the AHA Protocol. In an effort to stick with the AHA guidelines, in the left branch of the cardiac arrest algorithm, epinephrine is given after the 2nd shock during CPR and Amiodarone is given after the 3rd shock during CPR.
Kind regards,
Jeff
fredk says
In question 2, if bystander was already giving CPR, why wouldn’t you start with 1 mg epi IV?
Jeff with admin. says
As an EMS provider, you would start at the top of the algorithm with CPR and progress from there. Note question included starting an IV which would be needed prior to giving epinephrine. If you had more than two EMS providers, some of these interventions would take place at the same time. However, it is good to note the order of sequence so as to ensure providing the most important interventions first. Kind regards, Jeff
stasmi14 says
Hi Jeff,
Question #3- Ask while you are performing 5cycles of CPR, what other tasks can you be performing?
The answer was All of the above. But if I’m performing 5cycles of CPR, I can’t start an IV, open airway, etc…
Could you clarify this question?
Thank you, Stacie
Jeff with admin. says
In all of the scenarios, you can assume that you have a team of people working with you unless otherwise indicated in the scenario. This scenario assumes that there are other people available who will start IV, open the airway, etc.
Kind regards,
Jeff
Stacy ACLS says
question # 3
If the scenario assumes that there are other people available who will start IV, open the airway, etc.
Why would the question say?
While YOU are giving 5 cycles of CPR YOU! (ONE PERSON) CAN ALSO! carry out what other activities? that is strange wording
why wouldn’t it say, While YOU are giving 5 cycles of CPR other certified team members can also carry out what other activities?
Is this a trick question?
Is this how they ask questions on the exam?
everyone is telling not to worry but when I see thing like this with strange wording it makes me a bit nervous.
Jeff with admin. says
In the beginning of the scenario, it states, “The EMS team arrives shortly, takes over CPR, and attaches a defibrillator.”
Since the scenario indicates that there is an EMS team on the scene, the scenario assumes that the team is fully participating in the scenario.
I can see how the word “you” might throw someone off. I have changed this now to state “the team”
All the questions on this website are meant to help you prepare for certification. None of the questions are meant to be tricky or cause confusion.
I apologize for the confusion that you experienced. Thank you for the feedback.
Kind regards,
Jeff
anorden says
Hi Jeff,
In the ACLS bradycardia algorithm, it says to try atropine, and then if atropine is ineffective, to try TCP or dopamine or epi gtt. In this scenario is atropine not considered because the rhythm is complete block and therefore atropine would likely be ineffective? Technically (for the purposes of passing a written test) would atropine be a choice…although in real life if you recognize complete block or second degree type II (mobitz) you would go straight for TCP or dopa or epi.
Thanks so much – excellent site.
Jeff with admin. says
Your statement is correct. Atropine will likely be ineffective for 3rd degree block. However, for the purposes of passing the written test, AHA has been know to demand a rigid following of the algorithms.
Kind regards,
Jeff
natasha says
Question no 15 states that the patient is not breathing, has a faint pulse with hypotension and bradycardia.Here the hypoxemia may be causing these symptoms/signs.So why not treat it as a repiratory arrest and the intubate.
The bradycardia could be secondary to hypoxemia, so why should we follow the bradycardia algorithm.
I also agree the ECG shows a CHB.But kindly resolve this confusion.
Jeff with admin. says
In this scenario at question 15, the patient is attached to the difib. Montor and pacing can be easily stated quite rapidly to correct the perfusion issues that can be related to complete heart block. Also, this was a witness collapse and the rhythm was asystole upon arrival of EMS. The most common cause of witnessed collapse is cardiac arrest and therefore, respiratory arrest would not be considered a cause. I agree that after pacing, during the post arrest phase, intubation would be high on the list of priorities.
Kind regards,
Jeff
sstone says
I mean really your going do CPR & then you going to start an IV, give 02 support airwary – I mean if you had said 2 people on EMS but it said YOU come upon a person…. that is a lot to do when you are doing 5 cycles of 100 compressions …..by yourself ???? I really must be slow
Jeff with admin. says
Thanks for pointing this out. I have clarified the question. I agree that it is a little unreasonable to expect one person to do all this at once.
Kind regards,
Jeff
mailme.heather@gmail.com says
Just a thought, it would be helpful to have the rationale appear (particularly if you answer wrong) so that right away you can understand why the answer is not correct. Love the site so far-just getting into it. Thank you Jeff
Jeff with admin. says
Thank you for the suggestion. This is something that I do plan on implementing in the megacode scenarios once the new 2015 guidelines are released in early 2016.
Kind regards,
Jeff
rrt student says
On #17 Why not atropine as well?
Jeff with admin. says
The patient remains unstable, the pacer is already attached and the block is complete block. In a situation like this with unstable bradycardia, transcutaneous pacing would be the easiest way to control the heart rate. TCP is easy to start and easy to stop. It would be more prudent to stick with electrical pacing and stabilize the patient since the pacer is already attached to the patient and ready to go.
Kind regards,
Jeff
PeaKay says
scenario 3 question 7….is it assumed that CPR was resumed after epi given? I wanted to say resume CPR before the next shock so that epi circulates.
Mintoa says
Scenario 3 Q 15: Why initiate TCP instead of admin atropine?
Jeff with admin. says
The patient is post arrest, clinically unstable, and the defibrillator monitor is already attached. The best option is to initiate transcutaneous pacing. Also, the use of atropine may not be effective for 3rd degree block. AHA ACLS provider manual pg. 111 “Atropine administration should not delay implementation of external pacing for patients with poor perfusion.”
Kind regards,
Jeff
va student says
questiion 9, why check rhythm. I thought when performing VF, it is not necessary to check rhythm.
Jeff with admin. says
The rhythm check occurs after each round of CPR. For the cardiac arrest algorithm, you will always perform a rhythm check after completing 5 cycles of CPR.
Kind regards,
Jeff