 Tachycardia/tachyarrhythmia is defined as a rhythm with a heart rate greater than 100 bpm.
Tachycardia/tachyarrhythmia is defined as a rhythm with a heart rate greater than 100 bpm.
An unstable tachycardia exists when cardiac output is reduced to the point of causing serious signs and symptoms.
Serious signs and symptoms commonly seen with unstable tachycardia are: chest pain, signs of shock, SOA (short of air), altered mental status, weakness, fatigue, and syncope.
One important question you may want to ask is: “Are the symptoms being caused by the tachycardia?” If the symptoms are being caused by the tachycardia treat the tachycardia.
Causes
There are many causes of both stable and unstable tachycardia and appropriate treatment within the ACLS framework requires identification of causative factors. Before initiating invasive interventions, reversible causes should be identified and treated.
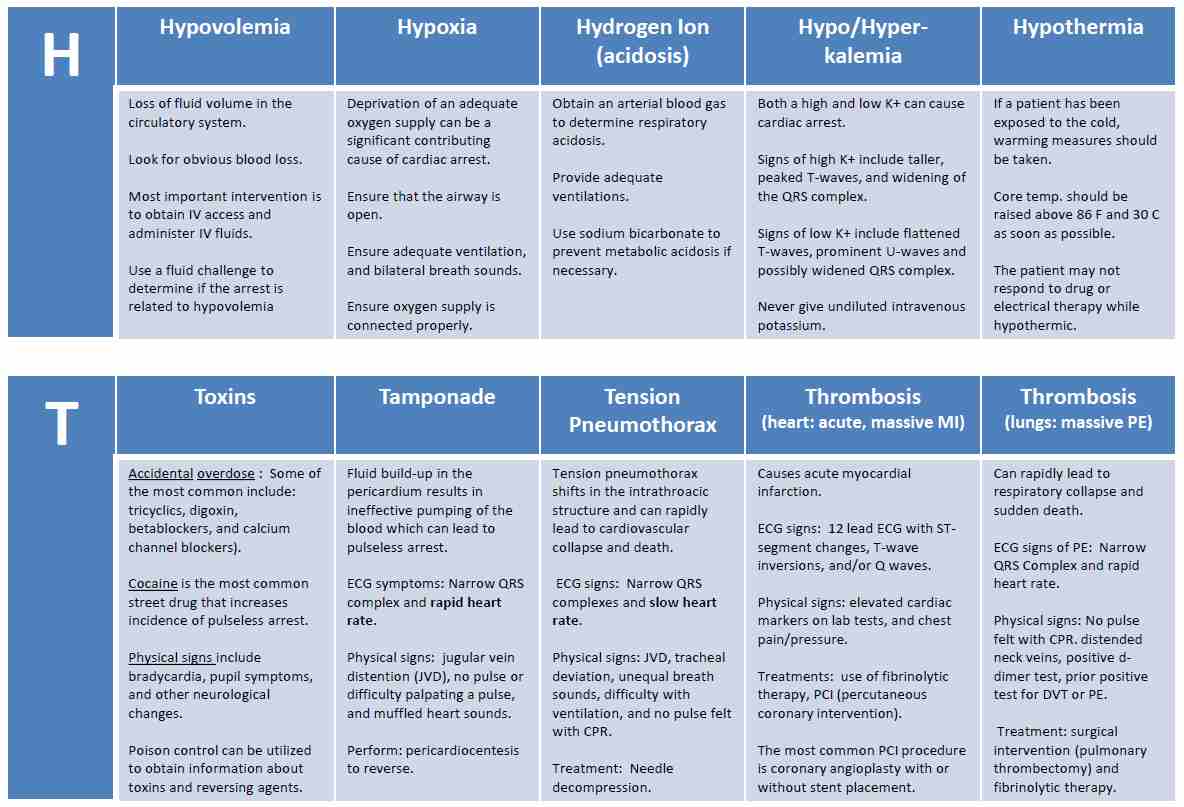
The most common causes of tachycardia that should be treated outside of the ACLS tachycardia algorithm are dehydration, hypoxia, fever, and sepsis. There may be other contributing causes and a review of the H’s and T’s of ACLS should take place as needed.
Click below to view the H and T’s table. When done click again to close the diagram.
H’s and T’s Table
Administration of OXYGEN and NORMAL SALINE are of primary importance for the treatment of causative factors of sinus tachycardia and should be considered prior to ACLS intervention.
Once these causative factors have been ruled out or treated, invasive treatment using the ACLS tachycardia algorithm should be implemented.
Associated Rhythms
There are several rhythms that are frequently associated with stable and unstable tachycardia these rhythms include:
- Supraventricular tachycardia (SVT)
- Atrial fibrillation
- Atrial flutter
- Monomorphic VT
- Polymorphic VT
- Wide-complex tachycardia of uncertain type
ACLS Treatment for Tachycardia
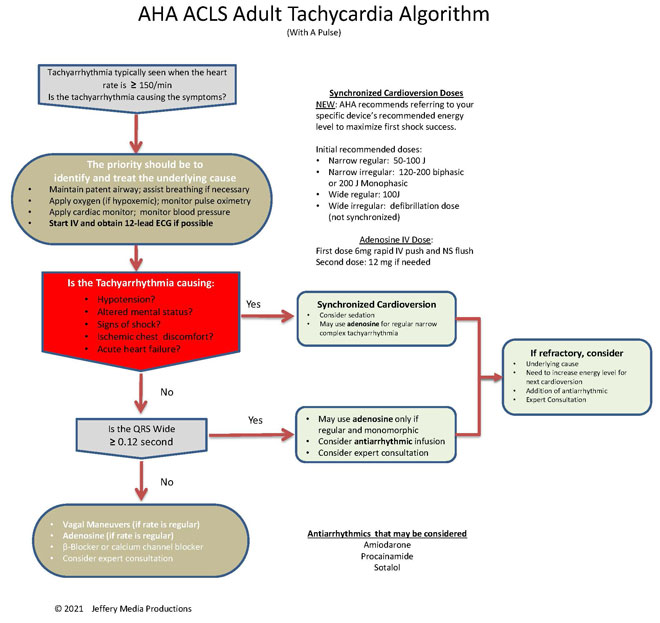
Click below to view the tachycardia algorithm diagram. When done click again to close the diagram.
Tachycardia Diagram
or Members Download the Hi-Resolution PDF Here(This will open in another window.)
The first question that should be asked when initiating the ACLS tachycardia algorithm is: “Is the patient stable or unstable?” The answer to this question will determine which path of the tachycardia algorithm is executed.
Unstable Tachycardia
Patients with unstable tachycardia should be treated immediately with synchronized cardioversion. If a pulseless tachycardia is present patients should be treated using the cardiac arrest algorithm.
The AHA no longer provides specific shock dose recommendations for synchronized cardioversion. Instead, they instruct to refer to your specific device’s recommended energy level to maximize first shock success.
For the purposes of a basic understanding of cardioversion, the information about general shock dosages and recommendations will remain in the content on this website.
The initial recommended synchronized cardioversion voltage doses are as follows:
- narrow regular: 50-100 J; i.e., SVT and atrial flutter
- Narrow irregular: 120-200 J biphasic or 200 J monophasic; i.e., atrial fibrillation
- Wide regular: 100 J; i.e., monomorphic VT
- Wide irregular: defibrillation dose (not synchronized)
Stable Tachycardia
Patients with stable tachycardia are treated based upon whether they have a narrow or wide QRS complex. The following flow diagram shows the treatment regimen for stable tachycardia with narrow and wide QRS complex.
- Stable (narrow QRS complex) → vagal maneuvers → adenosine (if regular) → beta-blocker/calcium channel blocker → get an expert
- Stable (wide/regular/monomorphic) → adenosine → consider antiarrhythmic infusion → get an expert
Dr.Hameed Chaudhari; Latur;India says
Sir;
Many times its difficult to differentiate between Coarse V.Fib.from Polymorphic VT.
Will you please guide me how to differentiate it on emergent basis.
Jeff with admin. says
VF will always be pulseless and if the VT is pulseless then it would be treated in the same manner as VF so it would not matter if it is misidentified. The best way to learn to differentiate is to look at plenty of rhythm strips. Just remember the treatment for VF and pulseless VT of any kind is the same. Kind regards, Jeff
leigh says
What is the recommended treatment for torsades not terminated with mag?
Jeff with admin. says
The recommended treatment for torsades not terminated with magnesium is defibrillation and then following the standard tachycardia algorithm. If the patient is pulseless then follow the right branch of the cardiac arrest algorithm.
There are other things that can be considered but they are beyond the scope of ACLS. If you are interested, here is an article about the subject with some good info. The info on treating torsades is toward the bottom. Polymorphic VT
Kind regards,
Jeff
Leigh says
What is the anti-arrhythmic of choice for torsades since most have a risk of prolonged qt?
Jeff with admin. says
All of following is assuming your first line for cardiac arrest with a torsades rhythm is defibrillation. Amiodarone would would be a reasonable choice if magnesium has been given and torsades persists. There are times when these antiarrhythmics can cause the thing they are treating, and you would have to be vigilant to watch for any prolonged QT interval.
Kind regards, Jeff
Sarfaraz Ahmad says
Excellent discussions and jeff you are simply great. Thanks
Jeff with admin. says
So glad to help. Kind Regards, Jeff
sborowiak10 says
Hi Jeff, I have a few questions regarding the tachycardia algorithm.
First, what would lead one to choose diltiazem over a beta blocker for rate control and what is the dosing for diltiazem? Second, is the beta blocker of choice going to be sotalol or metropolol? Third, is lidocaine still part of ACLS protocol?
Thank you in advance for your time!
Jeff with admin. says
Either can be used and will have similar effects. The link below is to information on the AHA position for use of calcium channel blockers (cardizem) and beta blockers. There is not much informaton that shows any significant difference between the use of either calcium channel blockers and beta-blockers. (the dosing for these medications is in the linked article below)
AHA position on calcium channel blockers and beta blockers
In my experience, if a physician trys one and it does not work then they will try the other. Different people definitely respond in different ways to each.
There will be no significant difference whether you choose sotolol or metoprolol. Througout my career, I have seen metoprolol used more frequently than sotalol.
Yes, lidocaine is still part of ACLS protocol but it is used as an alternative antiarrhythmic when amiodonare is not avaliable.
Here is the AHA position on lidocaine:
Kind regards,
Jeff
abosuyonov says
Hello Jeff.
What’s the treatment for stable polymorphic VT?
Jeff with admin. says
Polymorphic VT will not be stable for long because it most likely will not be providing adequate blood perfusion. The most common treatment for polymorphic VT whether stable or unstable IV magnesium. If unstable provide high energy unsynchronized shock.
Kind regards,
Jeff
Jas says
Hi Jeff, what are the common beta blockers and calcium channel blockers that we can give to patients with narrow qrs complex? And how do we prepare and give the medication? Thanks
Jeff with admin. says
One of the most common IV beta blockers in use today is Labatelol.
One of the most common calcium channel blockers in use today is Cardizem
Kind regards,
Jeff
Jas says
Thanks for the response Jeff. I have another question, Do we give them IV Bolus for tachycardia?
Jeff with admin. says
They can be given IV bolus and they can also be given as an infusion, It just depends upon the situation. If you have a situation where a bolus dose is not keeping the rate under control then a continuous infusion would be implemented to maintain inappropriate heart rate.
Kind regards,
Jeff
Mike Helms says
Is procanimide still used in acls usage
Jeff with admin. says
Yes, procainamide may be used in the treatment of wide complex tachycardia. See Pg. 168 of the AHA ACLS provider manual. This is the AHA guideline statement “Procainamide can be administered at a rate of 20 to 50 mg/min until the arrhythmia is suppressed, hypotension ensues, QRS duration increases >50%, or the maximum dose of 17 mg/kg is given. Maintenance infusion is 1 to 4 mg/min. Procainamide should be avoided in patients with prolonged QT and congestive heart failure.”
Kind regards,
Jeff
jas says
Hi Jeff, How much Diluent do we used For Procainamide and Sotalol infusion For Wide complex Tachycardia? thanks
Jeff with admin. says
Procainamide minimum dilution & dose: 1 g diluted to 50 mL with 5% Dextrose Injection may be administered at 17 mg/kg given with a max rate of 50 mg/min, or 100 mg over 2 minutes every 5 minutes until conversion. (from package insert)
Sotolol minimum dilution: Dilute in NS, D5W, or LR. Prepare in a volume of 100-250 ml. (minimum amt. 100 ml). The recommended initial dose of intravenous sotalol is 75 mg infused over 5 hours, once or twice daily based on creatinine clearance. The dose may be increased in increments of 75 mg/day every 3 days. The usual therapeutic effect is observed with oral doses of 80 to 160 mg once or twice a day (corresponding to 75 to 150 mg intravenous sotalol). Oral doses as high as 240-320 mg once or twice a day (corresponding to 225 to 300 mg intravenous sotalol) have been utilized in patients with refractory life-threatening arrhythmias. (from package insert)
Kind regards,
Jeff
madambac12 says
Another question from american heart association is a 53-year-old woman with has shortness of breath, chest discomfort, and weakness. The patient’s blood pressure is 102/59, the heart rate is 230/min, resp rate is 16 breaths/min. A patent peripheral iv is in place. What is the next action? ( The strip shows svt)
The correct answer is vagal maneuvers. The other answers were procedural sedation which was what I was originally leaning towards since patient might need synchronized cardioversion.
I’m conflicted because the vitals are somewhat stable except for the 230 heart rate, but the clinical signs and symptoms show unstable tachycardia. I somewhat understand the answer because her vitals are stable, but at the same time her clinical picture isn’t. If provided with conflicting information, do you base your decision on vitals or clinical picture? Thank you.
Jeff with admin. says
The only thing in the assessment that would indicate that the patient is unstable are the words “chest discomfort.” Other than that wording, this patient would qualify for vagal maneuvers and then adenosine if vagal maneuvers were unsuccessful. A heart rate of over 200 is typical for SVT and there is a good possibility that vagal maneuvers or adenosine would convert the rhythm to sinis rhythm.
Kind regards,
Jeff
madambac12 says
Thanks for your reply Jeff,
but you had written previously that
“Serious signs and symptoms commonly seen with unstable tachycardia are: chest pain, signs of shock, SOA (short of air), altered mental status, weakness, fatigue, and syncope”
This patient had 3 of these serious symptoms of unstable tach
Jeff with admin. says
I took a look at this scenario again. I saw the respirations of 16. I did not see where it said short of breath the first time. It doesn’t make sense to me why the respirations would be 16 and the patient would be short of breath. Do you expect the respirations to be out of the norm.
Weakness would not typically be associated directly with an unstable condition. To be honest the symptoms (chest discomfort and shortness of breath) make the question a little more difficult to interpret.
If I were them, I would change the symptoms this to make it more clear whether this is a stable or unstable condition.
It is not clear by the scenario whether the patient is truly stable or unstable. I would tend to think that the patient was stable because the blood pressure is stable.
Kind regards,
Jeff
madambac12 says
I was doing the acls preassessment test and came across this question.
A 45 year old woman with a history of palpitations develops light headedness and palpitations. She has received adenosine 6 mg iv for the rhythm (svt) shown here without conversion of the rhythm. She is now extremely apprehensive. Her blood pressure is 128/70 mmhg. What is the next appropriate intervention. ?
The answer is adenosine 12 mg Iv. Can you please explain why. I thought it would be vagal maneuvers since it had a narrow qrs and she seemed stable.
Thanks
Jeff with admin. says
This is a poorly worded question with no history of what was done prior to the administration of the first 6mg of adenosine.
Any attempt at vagal maneuvers should have been attempted prior to the administration of adenosine and this should have been made clear in the question. Vagal maneuvers is attempted before moving to adenosine. This is the order: vagal maneuvers → adenosine 6 mg → adenosine 12 mg. It is not in the AHA guidelines any more but it is still common practice to give a 2nd dose of 12 mg of adenosine if necessary.
Kind regards,
Jeff
bmuhr11 says
What is the dose for sotalol and procainamide if amiodarone is not a option?
Jeff with admin. says
AHA does not have a set recommended dose for procainamide at this time. There have been a couple of studies and AHA literature states that “procainamide can be given only as a controlled infusion (20 mg/min) because of its hypotensive effects and risk of QT prolongation, making it difficult to use during cardiac arrest.” Prolonged QT interval means that there is delayed repolarization of the heart following a heartbeat. Delayed repolarization can increase the risk for torsades de pointes and VF.)
Also stated is “One randomized comparison found procainamide (10 mg/kg) to be superior to lidocaine (1.5 mg/kg) for termination of hemodynamically stable monomorphic VT.390 Procainamide can be administered at a rate of 20 to 50 mg/min until the arrhythmia is suppressed, hypotension ensues, QRS duration increases >50%, or the maximum dose of 17 mg/kg is given. Maintenance infusion is 1 to 4 mg/min” ECC and CPR Guidelines, Part 7
Sotalol dosing also has not been concretely established. Here is the AHA statement about sotalol. “IV sotalol (100 mg IV over 5 minutes) was found to be more effective than lidocaine (100 mg IV over 5 minutes) when administered to patients with spontaneous hemodynamically stable sustained monomorphic VT in a double-blind randomized trial within a hospital setting.391 In a separate study of 109 patients with a history of spontaneous and inducible sustained ventricular tachyarrhythmias, infusing 1.5 mg/kg of sotalol over ≤5 minutes was found to be relatively safe and effective, causing hypotension in only 2 patients, both of whom responded to IV fluid.392 Package insert recommends slow infusion, but the literature supports more rapid infusion of 1.5 mg/kg over 5 minutes or less. Sotalol should be avoided in patients with a prolonged QT interval.” ECC and CPR Guidelines, Part 7
lailuma joyan says
112mg iv
KKBKONE says
how do you treat a stable VENTRICULAR TACHYCARDIA with pulse ,which algorithm and those with unstable VT and with pulse.
Jeff with admin. says
You would use the tachycardia algorithm to treat both stable and unstable ventricular tachycardia with a pulse. Kind regards, Jeff
Meg Rumsey says
my father in law has been admitted today following multiple VT episodes that have been seen at a routine pacing clinic.. the longest is 4.5 mins long . His echo is unremarkable . He has been feeling grotty and SOB after feeling his heart race occasionally over the past month but otherwise clinically very well… no routine meds.
U&Es normal.
Is there some sort of ablation or how else would this intermittent self limiting VT be treated ?
Thank you
Jeff with admin. says
Hi Meg,
This website is designed for helping health care providers prepare for advanced cardiac life support and it not the right place for me to answer medical questions. Here is a link to a good article about the treatments options for ventricular tachycardia. Kind regards, Jeff
DSW says
Hi Jeff
Just want to make sure I understand: Adenosine is used for narrow regular & and wide regular QRS complex tachycardia, and not Amiodarone for just regular wide QRS complex tachycardia?
Thanks,
DSW
Jeff with admin. says
Adenosine can be used for both narrow and wide complex tachycardia as long as the rhythm is regular. Amiodarone is normally reserved for ventricular arrhythmias. Please let me know if you have any other questions.
Kind regards,
Jeff
Roxanneang says
I’ve just read under the polymorphic ventricular tachycardia which is unstable that we treat with unsynchronised shocks because synchronisation is not possible. What does it mean when we have to treat unstable tachycardia with synchronised shocks as what was mentioned and highlighted from above. Thanks
Jeff with admin. says
Here is a page from the site that explains the difference between synchronized and unsynchronized cardioversion:
Synchronized vs. Unsynchronized Cardioversion
Kind regards,
Jeff
Murphles says
this link no longer seems to be working. Thanks.
Jeff with admin. says
Thank you for pointing this out. I have corrected the link. Kind regards, Jeff
manta51 says
What is the treatment of a stable wide/irregular/ polymorphic tachycardia? Is it only expert consultation only?
Jeff with admin. says
I don’t think I have ever seen this occur.
The appropriate intervention/treatment would be the following:
Kind regards,
Jeff