
SVT is a broad term for a number of tachyarrhythmias that originate above the ventricular electrical conduction system (Purkinje fibers).
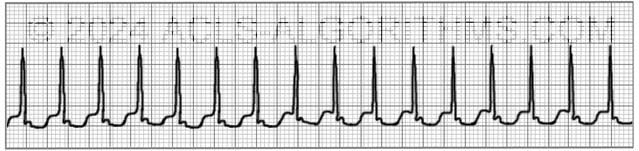
Classic Paroxysmal SVT has a narrow QRS complex & has a very regular rhythm. Inverted P waves are sometimes seen after the QRS complex. These are called retrograde p waves.

The heart fills during diastole, and diastole is normally 2/3 the cardiac cycle. A rapid heart rate will significantly reduce the time which the ventricles have to fill. The reduced filling time results in a smaller amount of blood ejected from the heart during systole. The end result is a drop in cardiac output & hypotension.
With the drop in cardiac output, a patient may experience the following symptoms. These symptoms occur more frequently with a heart rate >150 beats per minute:
- Shortness of air (S)
- Palpitation feeling in chest (S)
- Ongoing chest pain (U)
- Dizziness (S)
- Rapid breathing (S)
- Loss of consciousness (U)
- Numbness of body parts (S)
The pathway of choice for SVT in the tachycardia algorithm is based on whether the patient is stable or unstable. The symptoms listed above that would indicate the patient is unstable are noted with the letter (U). Stable but serious symptoms are indicated with the letter (S).
Unstable patients with SVT and a pulse are always treated with synchronized cardioversion. The appropriate voltage for cardioverting SVT is 50-100 J. This is what AHA recommends and also SVT converts quite readily with 50-100 J.
Below is a short video which will help you quickly identify supraventricular tachycardia on a monitor.
Please allow several seconds for the video to load. (4.37 mb)
Click for next Rhythm Review: Atrial Flutter
Questions Asked On This Page
-
Q: What are vagal maneuvers?
A: A vagal maneuver is a technique by which you attempt to increase intrathoracic pressure which stimulates the vagus nerve. This can result in slowed conduction of electrical impulses through the AV node of the heart. The following methods can be used.- Cough Method: Have a patient cough forcefully. This is a simple form of vagal maneuver. A cough stimulates an increase in intrathoracic pressure which will stimulate the vagus nerve. This can result in slowed conduction of electrical impulses through the AV node of the heart.
- Straw Method: Have the patient blow forcefully through a straw for 3-5 seconds.
- Bear down Method: Have the patient bear down and strain. Kind of like how a person might strain when having a bowel movement.
- Syringe Plunger Method: First, show the patient how easy it is to move the plunger by pulling it back and forth in within the syringe. Now instruct the patient place their mouth over the exit end of the syringe and attempt to blow the plunger out of the syringe. Have them blow for 3-5 seconds.
- Abdominal Pressure Method: Press into the patient’s abdomen while they contract and resist pressing into their abdomen.
- Ice Method: Quote from a healthcare provider: “We had a kid (approximately 12 yrs old) present to our ER in SVT, instead of using drugs and vagal maneuvers we dunked his face in a bucket of ice twice, and it immediately & effectively brought the heart rate down. We observed him for a period of time, and the kid was fine. Worked wonders! Young army doctor’s idea!”
-
Q: I can’t distinguish the sinus tachycardia example from the three re-entry SVT examples on the pre-test no matter how long I stare at the strips…they look identical to me. Help please, and thanks.
A: On the Pretest at the AHA website, Look at each image carefully. Don’t try to over-observe. Just look at each one and notice how many QRS complexes there are.
There are almost double the amount of QRS complexes in all of the SVT when compared to the Sinus Tachycardia. This is the easiest way to tell SVT from Sinus tachycardia. Also, P-waves are only clear in the sinus tachycardia. Most of the time with SVT you will not be able to see the p-waves. SVT rate will usually be greater than 150 and Sinus tachycardia will be less than 150. -
Q: Let me get this straight. Svt is a heart rate greater than 150 with conduction at or above the av node?
A: That is correct.
Regan says
I’m just learning. I work in a cardiologist office and we have a patient that had been to the emergency room with a heart rate in the 170’s Her ekg showed atrial flutter.
She was unconscious and the doctor I work for says whether atrial flutter/ svt it would not make a patient unconscious. I have to admit this is the first I’ve actually heard a patient being unconscious but is it really possible? There were no drugs in her system as all were negative.
Jeff with admin. says
There are instances where atrial flutter or SVT could make a patient become unconscious. That is possible. If a patient has new onset atrial flutter or SVT and they become unconscious and you cannot determine any other cause for the unconsciousness, it would be logical and acceptable to associate the cause of the unconsciousness with the atrial flutter or SVT until proven otherwise.
Kind regards,
Jeff
Sonia says
PAT symptomatic what is the acls treatment, is it cardioverion oor adenosine?
Jeff with admin. says
PAT is a form of SVT which originates within the atria but outside of the sinus node. Atrial flutter and multifocal atrial tachycardia are specific types of atrial tachycardia.
If a patient is symptomatic and UNSTABLE then the treatment would be cardioversion.
If a patient is symptomatic and STABLE then the treatment would vary depending of the cause of the PAT. In many cases, PAT will be asymptomatic and needs not treatment. However, in other cases such as toxicity, caffeine, or scarring on the heart. There are different treatments for each.
Kind regards,
Jeff
okto says
i’ve read some literature, the atrial tachycardia were classified as psvt and svt, how to differenciate them? or is it just the same?
Jeff with admin. says
Technically atrial tachycardia is different from SVT when it comes to SVT as presented within ACLS. When you think of arrhythmias, think of them in the two categories.
1. Arrhythmias above the ventricles (supraventricular)
2. Arrhythmias in the ventricles
SVT is a very generic term and within the framework of ACLS (I wish AHA would be more specific), SVT for ACLS purposes is typically referring to AVNRT and AVRT.
Atrial tachycardia is a type of SVT because it is supraventricular in nature, but because of the general nature of the word SVT and how the AHA ACLS provider manual uses the word, it can be confusing.
This can get a bit technical and so I have provided a link to a great article about SVT that may hopefully help clarify things for you.
Supraventricular Tachycardia Explained
I hope this helps.
Kind regards,
Jeff
Sunishvv says
Very use full
David says
Is there a way to distinguish between atrial tachycardia and SVT? I know AT is a form of SVT, however, i was taking a practice test for my NREMTP and was given a rhythm strip for interpretation… HR 170 regular narrow QRS, p waves buried in the T wave… I chose SVT, but the answer said AT.
Jeff with admin. says
It can be difficult to distinguish between AT and SVT. Here are two things that may help.
I hope this helps.
Kind regards,
Jeff
madambac12 says
I’m still having difficulty differentiating between stable and unstable patients. In the intro, you state
“An unstable tachycardia exists when cardiac output is reduced to the point of causing serious signs and symptoms.
Serious signs and symptoms commonly seen with unstable tachycardia are: chest pain, signs of shock, SOA (short of air), altered mental status, weakness, fatigue, and syncope”
Yet in the svt section, you differentiate between stable and unstable.
Shortness of air (S)
Palpitation feeling in chest (S)
Ongoing chest pain (U)
Dizziness (S)
Rapid breathing (S)
Loss of consciousness (U)
Numbness of body parts (S)
So a person who is short of air, palpitation feeling in chest, rapid breathing, dizziness, and numbness of body parts is considered stable?
Can you please clarify. thanks!!
Jeff with admin. says
Yes, a person who is short of air, palpations, rapid breathing, dizziness, and numbness and could be considered stable with SVT. The reason is that this type of SVT.
Typically unstable SVT and in fact any type of unstable tachycardia will involve chest pain, hypotension and changes in LOC.
Kind regards,
Jeff
Austin says
Level of conciousness is the biggest tell tale
eman salama says
Thank you for the very usefull and interactive discussion
Jeckson Mureri says
You have explained SVT, thanx J,
can you also help me in identifying & distinguishing polymorphic and monophonic tachycardia they confuse me a lot
Jeff with admin. says
Here is a web page that outlines both of these rhythms: Monomorphic and Polymorphic VT
Kind regards,
Jeff
cardisusu says
Does SVT- AVNRT and AVRT need to EP study? when? and successful rate?
Jeff with admin. says
Persistent SVT will probably require an electrophysiology study to determine the mechanism of the disorder. This will allow for proper treatment of the arrhythmia.
Kind regards,
Jeff
johannarocco says
What are vagal maneuvers?
Jeff with admin. says
A vagal maneuver is a technique by which you attempt to increase intrathroacic pressure which will stimulate the vagus nerve. This can result in slowed conduction of electrical impulses through the AV node of the heart. There are a number of ways to do it here are a couple:
Hope this helps. Kind regards, Jeff
johannarocco says
It’s a great help Jeff.
Thank you so much.
Les says
I have used this method myself at home numerous times to slow a tachy heart rate. Cold tap water with no ice in the bathroom sink worked well, due to the body’s natural reaction to protect itself from drowning (all body systems slow down when the body or even face is submerged in water).
ChrisL says
If pt has not converted after vagaries man. and has had a total of 18mg of Adenosine admin per our protocol, should we consider cardioverting? Or monitor pt en route and call MD at receiving facility for consultation?
Jeff with admin. says
At this stage, a cardiologist should be involved in the next treatment options. As long as the patient is stable, this would be the case. At any point if the patient becomes unstable you would perform cardioversion.
Kind regards,
Jeff
Toni says
Can you call PAF and PAT—SVT?
Jeff with admin. says
Yes, premature atrial tachycardia (PAT) would be considered a of supraventricular tachycardia. Not sure what you mean by PAF, but if you mean atrial fibrillation with a rapid ventricular rate then yes, this would also fit the criteria for SVT.
Kind regards,
Jeff
Michaela says
We usually refer : PAT and PAF as paroxysmal atrial tach and paroxysmal atrial fibrillation when the event starts suddenly, and many SVT events do start suddenly
Maureen Parish says
How do you differenciate SVT from reentry SVT
Jeff with admin. says
The 4 most common types of SVT are A-V Nodal Reentry Tachycardia, A-V
Reentry Tachycardia, atrial tachycardia and atrial flutter. These rhythms are regular in nature and have a rate > 150. To distinguish the difference between the re-entry tachycardias and the other types really requires a 12 lead ECG. The diagnostic criteria to determine that it is a reentrant tachycardia is actually quite complex. I attached a pic from my 12 lead ecg pocket reference that will help. Reentry tachycardias are very easy to convert and often vagal maneuvers will suffice to terminate the tachycardia.
Kind regards,
Jeff
Linsey says
Lets say I have a pt hooked up to a basic tele monitor and she goes into SVT. Vagal maneuvers are attempted and doctor orders Adenosine. Would you then hook her up to the code cart prior to giving the Adenosine.?
Linsey says
Oh and the patient is in stable condition.
And would your answer be different if the patient had multiple reentrys into SVT and successful Adenosine administrations? Or maybe just having the code cart at bedside? Can Adenosine cause lethal arrhythmias?
Jeff with admin. says
The crash cart would not be necessary, but it could be close at hand in the case that the patient becomes unstable. Adenosine does not normally precipitate lethal arrhythmias.
Kind regards,
Jeff
Jeff with admin. says
Having the code cart prior to giving adenosine would not be necessary. It would not hurt, but it would not be necessary. Adenosine rapid IV push will not usually precipitate pulseless VT or VF.
Kind regards,
Jeff
Dana says
How can we treat svt in hypotensive patient <90 systolic , while refusing dc shock?
Jeff with admin. says
If the patient refuses cardioversion, you could attempt adenosine as prescribed for SVT in the AHA ACLS tachycardia algorithm. Kind regards, Jeff