 The major ECG rhythms classified as bradycardia include:
The major ECG rhythms classified as bradycardia include:
- Sinus Bradycardia
- First-degree AV block
- Second-degree AV block
- Type I —Wenckebach/Mobitz I
- Type II —Mobitz II
- Third-degree AV block complete block
Bradycardia vs. Symptomatic Bradycardia
Bradycardia is defined as any rhythm disorder with a heart rate less than 60 beats per minute. (Usually less than 60)
Symptomatic bradycardia, however, is defined as a heart rate less than 60/min that elicits signs and symptoms, but the heart rate is typically less than 50/min.
Symptomatic bradycardia exists when the following 3 criteria are present: 1.) The heart rate is slow; 2.) The patient has symptoms, and 3.) The symptoms are due to the slow heart rate.
Relative bradycardia occurs when a patient may have a heart rate within normal sinus range, but the heart rate is insufficient for the patient’s condition. An example would be a patient with a heart rate of 80 bpm when they are experiencing septic shock.
Bradycardia Pharmacology
There are 3 medications that are used in the Bradycardia ACLS Algorithm. They are atropine, dopamine (infusion), and epinephrine (infusion). More detailed ACLS pharmacology information is reviewed following this page.
- The single dose administration of atropine was increased from 0.5 mg to 1 mg. Now give 1 mg for the first dose and then repeat every 3-5 minutes at the 1 mg dose.
- Also, the dopamine infusion rate for chemical pacing was changed to 5-20 mcg/kg/min.
The previous rate from the 2015 guidelines was 2-20 mcg/kg/min. - The demand rate may be set at a range from 60-80/min. 2015 guidelines had the start demand rate to start at only 60/min.
2015 AHA Update: For symptomatic bradycardia or unstable bradycardia IV infusion a chronotropic agent (dopamine & epinephrine) is now recommended as an equally effective alternative to external pacing when atropine is ineffective.
Atropine: The first drug of choice for symptomatic bradycardia. The dose in the bradycardia ACLS algorithm is 1 mg IV push and may repeat every 3-5 minutes up to a total dose of 3 mg.
Dopamine: Second-line drug for symptomatic bradycardia when atropine is not effective. Dosage is 5-20 micrograms/kg/min infusion.
Epinephrine: Can be used as an equal alternative to dopamine when atropine is not effective. Dosage is 2-10 micrograms/min.
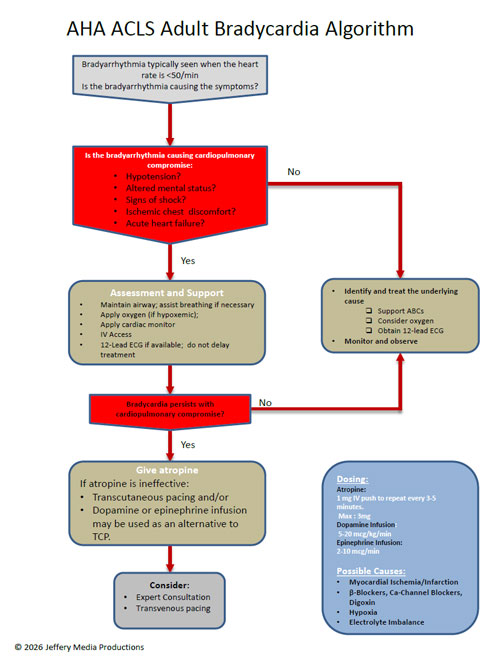
Bradycardia Algorithm
The decision point for ACLS intervention in the bradycardia algorithm is determination of adequate perfusion. For the patient with adequate perfusion, observe and monitor the patient. If the patient has poor perfusion, preparation for transcutaneous pacing should be initiated, and an assessment of contributing causes (H’s and T’s) should be carried out.
Click below to view the bradycardia algorithm diagram. When finished, click again to close the diagram.
Bradycardia Algorithm Diagram
or Download the High Resolution PDF Here. (This will open in another window.)
Transcutaneous pacing (TCP)
Preparation for TCP takes place as atropine is being given. If atropine fails to alleviate symptomatic bradycardia, TCP is initiated. Ideally, the patient receives sedation prior to pacing, but if the patient is deteriorating rapidly, it may be necessary to start TCP prior to sedation.
For the patient with symptomatic bradycardia with signs of poor perfusion, transcutaneous pacing is the treatment of choice.
Do not delay TCP for the patient with symptomatic bradycardia with signs of poor perfusion. The starting rate for TCP is 60-80/min and adjust up or down based on the patient’s clinical response. The dose for pacing is set at 2mA (milliamperes) above the dose that produces observed capture.
TCP is contraindicated in the patient with hypothermia and is not a recommended treatment for asystole.
Do not use a carotid pulse check for the assessment of circulation as TCP can create muscular movements that may feel like a carotid pulse. Assess circulation using the femoral pulse.
Identification of contributing factors for symptomatic bradycardia should be considered throughout the ACLS protocol since reversing of the cause will likely return the patient to a state of adequate perfusion.
Top Questions Asked on This Page
-
Q: Should I use atropine in all cases of symptomatic bradycardia regardless of the level of block? The prep test for AHA ACLS seems to support giving atropine initially in symptomatic second-degree block type II, but not for complete block.
A: There are a couple of things to mention here. First, atropine may be used for any type of block but may negatively affect outcomes if the bradycardia is being caused by myocardial infarction.
This negative effect may occur because atropine increases the heart rate and myocardial oxygen demand. In the case of bradycardia caused by MI, it would be safer to transcutaneous pace (TCP) at a rate of 60 and move toward some type of cardiac intervention. You should use the 12 lead ECG to help determine MI. This will help determine if atropine may exacerbate the patient’s condition. If the patient has severe symptoms, you should not delay transcutaneous pacing (TCP).
You will usually have time to try atropine as you prepare for TCP.
Second, AHA states “For Mobitz II and complete block (3rd Degree block), atropine should not be relied upon.” This does not mean that it is contraindicated. It just means that it should not be relied upon because there is a good chance that it will not work.
It may not work because atropine blocks the action of the vagus nerve. Atropine works at the SA and AV node through its effect on the vagus nerve, and since conduction abnormalities associated with 2nd-degree block type II and 3rd-degree heart block are below (distal) the site of action for atropine, the drug will typically have an insignificant effect.
-
Q: Why is pacing contraindicated in hypothermia?
A: Bradycardia may be physiologic in the hypothermic patient. This type of bradycardia is an appropriate response to the decreased metabolic rate that normally occurs with hypothermia.
Also the hypothermic ventricle is more prone to fibrillation with any sort of irritation. Thus the irritation of TCP could induce VF. Once the hypothermic ventricle begins to fibrillate, it is more resistant to defibrillation. Warm the patient and then treat any remaining arrhythmias.
-
Q: What is TCP?
A: TCP means transcutaneous pacing.
-
Q: What is chemical pacing?
A: Chemical pacing is when IV medications (epinephrine or dopamine) are used to increase the heart rate rather than the transcutaneous pacing which uses electricity to increase the heart rate.
Phinda Paramedic student says
Hi what is the maximum rate that u can set on the pacer is it 90 or 100 bpm regardless of the mA for electrical capture and which patient will this apply to as well as on which cardiac conditions would the maximum parameter have detrimental effects on.
Jeff with admin. says
Different defibrillators have different settings. I do not think that there is a standards maximum for the heart rate.
Most of the time you would start with the beats per minute set to 60 and titrate the beats per minute up until the patient is stable. I have not seen any patient that needed pacing greater than 80 bpm. There are a lot of factors that come into play (blood pressure, cardiac output, chest pain, etc.) and a lot of these factors would be what determines how a physician will respond to any given situation.
Kind regards,
Jeff
Kent says
If atropine increases firing from the SA node why couldn’t it theoretically be used in Asystole? And if I wished to give dopamine as a rapid IV/IO push rather than an infusion what dosage should I give?
Jeff with admin. says
Prior to 2010, atropine was part of the right branch of the cardiac arrest algorithm for the treatment of bradycardia PEA and asystole. After 2010, atropine was removed from the cardiac arrest algorithm because it had never been demonstrated that atropine improved outcomes.
There is a hypothetical justification for atropine based on physiology/pathophysiology, but this hypothetical justification has not shown to be of actual benefit for the patient experiencing cardiac arrest.
I have never seen any recommendations for the administration of dopamine rapid IV push. The plasma half-life of dopamine is about 2 minutes so the effects of dopamine would be very short-lived if given as a bolus IV push.
Dopamine is typically ordered as a weight-based drip infusion. I cannot get any recommendations for a dose for rapid IV push.
Kind regards,
Jeff
tfitzpatrick says
I noticed you recommend in TCPto set the rate at 60bpm and 2 mA above what you get capture at. In my 2015 ACLS hand book pg 17, it said to set the rate at apox 80 bpm, and makes not recommendation on mA, more than just what is needed for capture. what you recommend seems to make since but were are you getting your numbers
thanks
paramedic tyler
Jeff with admin. says
I’m not sure if you are looking at the 2015 AHA ACLS Provider Manual. Page 17 in the 2015 AHA ACLS Provider Manual has nothing to do with bradycardia or TCP.
On Pg. 127 of the AHA ACLS Provider Manual near the bottom of the page, it states: “Set the demand rate to approximately 60/min. This rate can be adjusted up or down once pacing is established.” Then it states: “Set the current milliamperes output to 2mA above the dose at which consistent capture is observed.”
Kind regards,
Jeff
dhellekson says
When would you start to consider pacing? After the first dose of atropine 0.5mg is note effective or the max dose of 3 mg not being effective. Thank you.
Jeff with admin. says
If the patient has poor perfusion you would begin considering external pacing before or during your first administration of atropine.
When a patient has signs of poor perfusion exterior pacing is the preferred treatment and atropine can be attempted as long as it does not delay the use of external pacing.
In most situations there will be multiple people available and the administration of atropine will not delay the use of external pacing and can be attempted.
Kind regards,
Jeff
Josh Swenson says
My protocol in Utah county advise for symtomatic bradycardia to administer 1 mg of Epi 1:10,000 for first round drug choice. I agree that Atropine should be first line. Would anyone know why my protocol would advise Epi for first line.
Jeff with admin. says
There are certain regions where different protocols are used. Sometimes this is research based and data is being collected on the use of medications in emergencies.
In other cases, these things are determined by a board of emergency professionals.
In other cases, the protocols are outdated and need correction.
A good question to ask your supervisor is “why don’t we follow the AHA ACLS guidelines for the treatment of symptomatic bradycardia?”
Kind regards,
Jeff
Reezwan says
What is the management of a patient in asystole due to complete heart block? Is there any role of atropine in complete heart block? Is there any role of ,
Bolus I/V Adrenaline in this scenario?
Jeff with admin. says
If the patient is in asystole, this means that there is no electrical impulse being generated from the heart and you see a flat line on the monitor. The treatment would be the right branch of the cardiac arrest algorithm which prescribes high-quality CPR with 1mg boluses of epinephrine (adrenaline) given every 3-5 minutes. Kind regards, Jeff
Reezwan says
Thanks Jeff. So, what kind of bradycardias are we supposed to is atropine in? As in which type of heart blocks?
Jeff with admin. says
Atropine can be used on any block. It is not contraindicated. However, it may not be effective for 2nd degree block type II and complete block. Also, if ischemia is suspected, you would want to be very cautious about using atropine. The increase in heart rate can worsen cardiac ischemia because of the increase work placed on the heart.
Kind regards,
Jeff
Reezwan says
Thanks Jeff
maheshkumarortho@gmail.com says
we have been using the simple technique of elevation the legs immediately while evaluating the condition or waiting for the emergency medical service for some one who had fainting attack or shock due to over exertion, pain shock etc., with the logic of -elevation of the legs will enhance the venous return and increase the diastolic filling thereby improve the cardiac output. And we have found useful in many occasions.
But this is not mentioned or discussed in any of the BLS or ACLS scenarios. I would like to know the effective ness of this technique. Is there any studies done to see the effectiveness of this procedure in ACLS scenarios?
Jeff with admin. says
In shock states this technique can be used and is based on sound evidence. More current research has focused on using this as a method to determine if a patient will respond to a fluid.
Here’s an article about this with references at the end:
Passive leg raising technique
Kind regards,
Jeff
maheshkumarortho@gmail.com says
What is the difference between pacing by external transcutaneous pacing and automated implanted pace maker in terms of pain during pacing and also in terms of survival?
Jeff with admin. says
External transcutaneous pacing can be quite uncomfortable because of the exposure to all of the nerves in the upper tissues. External transcutaneous pacing is not used for long-term treatment.
Regarding and internal pacemaker, after the initial surgery to implant the device, there is no pain involved with Implanted Internal automated pacemaker. The pacer wires are implanted directly into the heart muscle and therefore there is no pain sensed.
Kind regards,
Jeff
Vicky says
Which amperage is suggested to start with , during TCP?
Thank you,
Vicky
Jeff with admin. says
You start at 0J and increase the dose until you get capture. (Capture means that the external pacemaker has taken over and is delivering all the electrical impulses that are causing the heart muscle to contract.) Once you have capture, go up at least 2 mA. The machine will probably make you go up by increments of 5 mA. Kind regards, Jeff
Dr.Hameed Chaudhari; Latur;India says
What are guidelines to maintain the sinus rhythm in a patient of symptomatic Bradycardia who has responded to atropine?
Jeff with admin. says
If the patient with symptomatic bradycardia has responded with use of atropine then you can continue to use atropine to improve the condition of the patient. Atropine is the first line drug to be used with symptomatic bradycardia.
Kind regards,
Jeff
SchrollG says
Thanks so much for creating and maintaining this great web resource!
I work in cardiac rehab and have been procrastinating with RE-certification coming up. I just started studying 3 days ago using your website. My RE-certification test in on 11/28. I used your website when I first took ACLS 2 years ago. So far, I have made it through about 30% of your website material using the interactive guide. What advice could you offer me as far as how I prioritize study time until my test on 11/28?
Thanks!
Jeff with admin. says
It sounds like you are making good headway through the materials. I would recommend continuing with the interactive course guide and taking about 2-3 hours each day if you want to get through all of the materials on the site by 11/28.
Since you have taken ACLS before, you may not need to dedicate as much time to going through the written materials, but you will want to watch each video that is included in the sections of the interactive course guide. Taking notes on these videos may help reinforce the content in your mind as well.
Kind regards,
Jeff
Pandula says
what is the place for isoprenaline in symptomatic bradycardia?
European resuscitation guidelines 2015 recommend it as effective as adrenaline infusion as 5 ug/kg/min.
Jeff with admin. says
AHA does not classify Isoproterenol, and does not list it in the guidelines as a replacement for epinephrine or dopamine.
However, it does give the following recommendation:
“Isoproterenol is a β-adrenergic agent with β-1 and β-2 effects, resulting in an increase in heart rate and vasodilation. The recommended adult dose is 2 to 10 mcg/min by IV infusion, titrated according to heart rate and rhythm response.”
Here is the reference: Isoproterenol
Kind regards,
Jeff
Thomas says
Hi Jeff,
South African 3rd year BHSc: EMCR student here, studying at DUT.
Recently I had a simulation at varsity where the patient had an unstable bradycardia due to a 2nd degree Mobitz I. I misinterpreted the Mobitz I for a Mobitz II. Therefore I decided not to administer Atropine as I assumed it would be ineffective and as the patient was unstable (Hypoxic, hypotensive + unresponsive), I did not want to wait delay TCP/adrenaline. I decided to go for an adrenaline infusion 2mg/200ml Nacl @ 10mcg/min and the patient responded positively to my treatment and was stabilised. However I failed the simulation due to my misinterpretation and failure to provide 1st line treatment of atropine.
My questions are:
When in doubt about the 3-lead rhythm diagnosis (IE unsure between Mob I and II due to monitor interference + artifacts + lack of printable paper making P-waves difficult to distinguish), is it better to go with atropine over adrenaline/TCP?
If so, how many doses of Atropine should you administer (lets say it is a Mobitz II and the atropine is ineffective) before you move on to TCP/adrenaline? (taking into account that each dose brings with it a 3-5min delay from definitive treatment).
Lastly, in actual practice on real patients, how effective is atropine in treating Mobitz I? Due to the fact that in Mobitz I, the block occurs between the SA node and the AV node. As Atropine achieves it’s effects through stimulating the SA node to generate impulses, are these impulses not affected by the heart block? Thus making atropine less effective or even ineffective?
Best regards,
Thomas
Jeff with admin. says
The instructor was testing your knowledge. They were not wanting to know what you would do in a real scenario. They were wanting your to verbalize 1st line treatments that should be carried out in the ideal scenario. Here is why:
“Clinical trials in adults showed that IV atropine improved heart rate, symptoms, and signs associated with bradycardia.”
Here is the reference for that: Atropine in adults
Simply put Atropine is very effective when it works.
You should have verbalized it something like this “since atropine is a 1st line medication for treating bradycardia, let’s give 0.5 mg atropine while we prepare for TCP. We can give 0.5mg and see if we get a response.” If you get a response then you would know that you could give a 2nd dose and probably see more improvement. If you see no response to the 1st dose of atropine then move on to the next treatment promptly.
Mobitz 1 is typically benign and would not require treatment. However, patients with symptomatic bradycardia (Mobitz 1) typically respond well with the use of atropine.
Kind regards,
Jeff
Kevin says
Should atropine be used to treat high degree blocks such as Mobitz 2 or Third degree? My understanding is that atropine may not work in high degree blocks and can in theory make it worse, but I continue to find conflicting answers for if and when it should be administered. Some say it can be attempted while awaiting TCP, others say it is the first line med for all symptomatic bradycardia and then others say it will not work for high degree blocks. Is there a definitive answer?
Jeff with admin. says
I would say that there is not a definitive answer for this as there are a few instances where atropine might be effective. Here are a couple of interesting quotes:
Kind regards,
Jeff
Einar says
If we’re dealing with an MI, atropine could be detrimental by causing the heart muscle to work more, demanding more oxygen, and possibly increasing the size of the infarct. Once the drug is administered you can’t stop the effects. As for pacing, you can adjust the energy being delivered or even stop the pacer if patient starts deteriorating. Probably safer for the pt. Just my two cents
CS
Jeff with admin. says
Thanks for your comment. I agree with you. and to be honest, I’m not sure why American Heart Association hasn’t notified and guidelines to reflect this better. Kind Regards, Jeff
Kevin says
I understand that atropine should be used with caution in people with an ACS. Shouldn’t dopamine and epinephrine also be used with caution since both have inotropic and chronotropic effects that can potentially increase damage to the heart?
Jeff with admin. says
Yes, that is correct. Any medication (anything) that could increase the oxygen demand on the heart could potentially worsen the damage to the heart. The nice thing about epinephrine and dopamine is they have a short half-life and their effect diminish rapidly.
Kind regards,
Jeff