Lidocaine may be considered a suitable antiarrhythmic that can be used to treat cardiac arrest from VT/VF.
Lidocaine is now included in the AHA Cardiac Arrest diagram along with amdidoarne. Emphasis should not be on the use of medications and it is the AHA recommendation to place more emphasis on high quality CPR and early defibrillation.
Lidocaine indications for ACLS
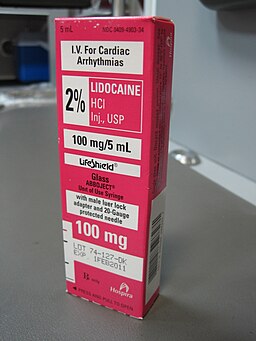
- In ACLS, Lidocaine is used intravenously for the treatment of ventricular arrhythmias. (VT/VF)
- It is also useful for the treatment of stable monomorphic VT with preserved ventricular function and for stable polymorphic VT with preserved left ventricular function, normal QT interval, and correction of any electrolyte imbalances.
The overall benefits of lidocaine for the treatment arrhythmias in cardiac arrest has come under scrutiny. It has been shown to have no short term or long term efficacy in cardiac arrest.
Routine prophylactic use is contraindicated for acute myocardial infarction.
Side Effects
Lidocaine should be used with caution due to negative cardiovascular effects which include hypotension, bradycardia, arrhythmias, and/or cardiac arrest. Some of these side effects may be due to hypoxemia secondary to respiratory depression.
Lidocaine Toxicity
Symptoms of lidocaine toxicity progress in the following predictable pattern. It begins with numbness of the tongue, lightheadedness, and visual disturbances and progresses to muscle twitching, unconsciousness, and seizures, then coma, respiratory arrest, and cardiovascular depression.
There are several conditions that increase the potential for lidocaine toxicity:
- Liver dysfunction increases the risk of toxicity due to lidocaine being metabolized by the liver.
- Low protein increases the risk of toxicity because lidocaine is protein bound.
- Acidosis can also increase the risk of toxicity since acidosis increase the potential of lidocaine to dissociate from plasma proteins.
Dosing
Cardiac Arrest from VT/VF:
- Initial dose: 1 to 1.5 mg/kg IV/IO
- For refractory VF may give additional 0.5 to 0.75 mg/kg IV push, repeat in 5 to 10 minutes; maximum 3 doses or total of 3mg/kg
Perfusing Arrhythmia:
For stable VT, wide-complex tachycardia of uncertain type and significant ectopy:
- Doses Range from 0.5 to 0.75 mg/kg and up to 1 to 1.5mg/kg
- Repeat 0.5 to 0.75 mg/kg every 5-10 minutes with maximum total dose of 3 mg/kg
Maintenance infusion:
- 1 to 4 mg/min (30-50 mcg/kg/min)
Discontinue a lidocaine infusion immediately if signs of toxicity develop.
Kaye says
Hello how to administer adrenaline? Diluted or undiluted?
How about magnesium can be given undiluted?
And lidocaine diluted or undiluted? If
All diluted how much each
ACLS says
In an ACLS emergency, adrenaline (epinephrine) should be administered diluted. For intravenous (IV) or intraosseous (IO) administration, the standard 1 mg dose of epinephrine should be diluted to a 1:10,000 concentration (0.1 mg/mL). This is typically achieved by diluting 1 mL of 1:1000 epinephrine with 9 mL of normal saline, resulting in a total volume of 10 mL.
Magnesium sulfate should not be given undiluted in ACLS emergencies; it must always be diluted before administration. The recommended dose of 1-2 grams should be diluted in 10 mL of D5W or normal saline and administered via slow IV or IO push over 5 to 20 minutes to prevent severe side effects.
Lidocaine should generally be diluted for administration in ACLS emergencies. When given intravenously or intraosseously, it is typically used in its standard concentration (e.g., 1% or 2%). However, if administered via an endotracheal tube, it must be diluted in 5–10 mL of normal saline or sterile water to ensure proper absorption and distribution.
Kind regards,
Jeff
Raymond Jeff Massay says
Thanks, particularly when the feeling that Lidocaine is “an old drug”, and the world only needs Amiodarone.
Jeff
Jason P. (MD) says
There’s a pretty interesting article circulating from CHEST demonstrating increased efficacy of lido in comparison to amiodarone for pulseless VTach/VFib arrest. (Wagner et. al, 2022) We’re talking statistically significant odds ratios of 1.15 for achieving ROSC and 1.19 for overall survival, with numbers in the study to provide pretty solid statistical power.
The disclaimer on Lido for pulseless VFib arrest (“The overall benefits of lidocaine for the treatment arrhythmias in cardiac arrest has come under scrutiny. It has been shown to have no short term or long term efficacy in cardiac arrest.”) might be out of date.
I’m curious to see when / if there will be an algorithm change.
Anyway, I just wanted to pass that along.
Cheers,
Jason
Here’s the article below. I have a hunch this is going to bring out some national changes in practice.
https://pubmed.ncbi.nlm.nih.gov/36332663/
ACLS says
Thanks Jason. That is interesting. It will be interesting to see what happens with the algorithm in 2025.
Kind Regards, Jeff
Marius says
In 2019 Wagner et al. also published in Circulation comparing Amiodarone vs Lidocaine. The outcomes was the same except for the 2019 publication said that Lidocaine compared to Amiodarone was not associated with higher ROSC rates.
https://www.ahajournals.org/doi/10.1161/circ.140.suppl_2.29
It would be interesting to see what the 2025 AHA Guidelines will recommended. I think Lidocaine might become the first choice.