 The major ECG rhythms classified as bradycardia include:
The major ECG rhythms classified as bradycardia include:
- -Sinus Bradycardia
- -First-degree AV block
- -Second-degree AV block
- -Type I —Wenckebach/Mobitz I
- -Type II —Mobitz II
- -Third-degree AV block complete block
Bradycardia vs. Symptomatic Bradycardia
Bradycardia is defined as any rhythm disorder with a heart rate less than 60 beats per minute. (Usually less than 60)
Symptomatic bradycardia, however, is defined as a heart rate less than 60/min that elicits signs and symptoms, but the heart rate is typically less than 50/min.
Symptomatic bradycardia exists when the following 3 criteria are present: 1.) The heart rate is slow; 2.) The patient has symptoms, and 3.) The symptoms are due to the slow heart rate.
Relative bradycardia occurs when a patient may have a heart rate within normal sinus range, but the heart rate is insufficient for the patient’s condition. An example would be a patient with a heart rate of 80 bpm when they are experiencing septic shock.
Bradycardia Pharmacology
There are 3 medications that are used in the Bradycardia ACLS Algorithm. They are atropine, dopamine (infusion), and epinephrine (infusion). More detailed ACLS pharmacology information is reviewed following this page.
- The single dose administration of atropine was increased from 0.5 mg to 1 mg. Now give 1 mg for the first dose and then repeat every 3-5 minutes at the 1 mg dose.
- Also, the dopamine infusion rate for chemical pacing was changed to 5-20 mcg/kg/min.
The previous rate from the 2015 guidelines was 2-20 mcg/kg/min. - The demand rate may be set at a range from 60-80/min. 2015 guidelines had the start demand rate to start at only 60/min.
2015 AHA Update: For symptomatic bradycardia or unstable bradycardia IV infusion a chronotropic agent (dopamine & epinephrine) is now recommended as an equally effective alternative to external pacing when atropine is ineffective.
Atropine: The first drug of choice for symptomatic bradycardia. The dose in the bradycardia ACLS algorithm is 1 mg IV push and may repeat every 3-5 minutes up to a total dose of 3 mg.
Dopamine: Second-line drug for symptomatic bradycardia when atropine is not effective. Dosage is 5-20 micrograms/kg/min infusion.
Epinephrine: Can be used as an equal alternative to dopamine when atropine is not effective. Dosage is 2-10 micrograms/min.
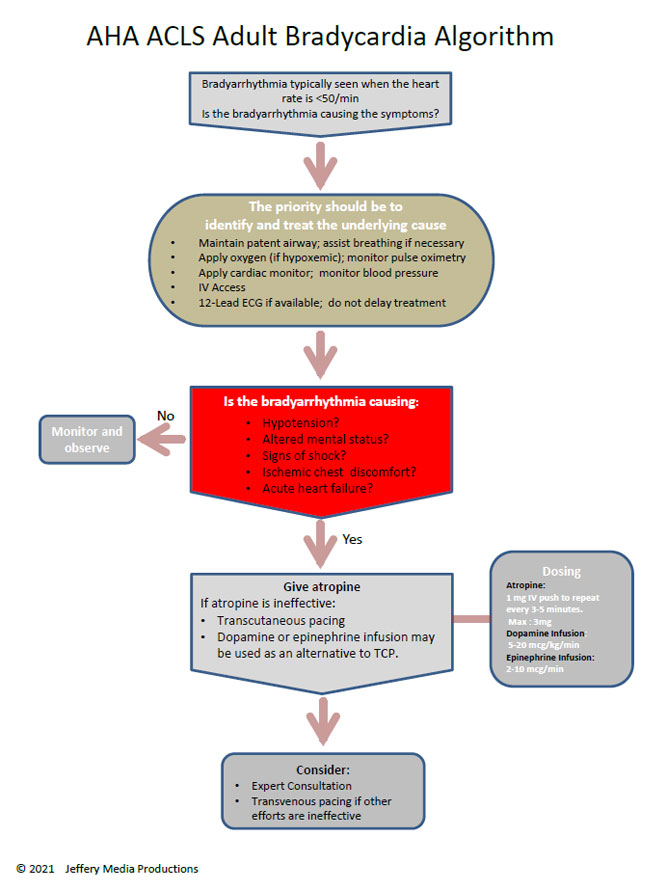
Bradycardia Algorithm
The decision point for ACLS intervention in the bradycardia algorithm is determination of adequate perfusion. For the patient with adequate perfusion, observe and monitor the patient. If the patient has poor perfusion, preparation for transcutaneous pacing should be initiated, and an assessment of contributing causes (H’s and T’s) should be carried out.
Click below to view the bradycardia algorithm diagram. When finished, click again to close the diagram.
Bradycardia Algorithm Diagram
or Download the High Resolution PDF Here. (This will open in another window.)
Transcutaneous pacing (TCP)
Preparation for TCP takes place as atropine is being given. If atropine fails to alleviate symptomatic bradycardia, TCP is initiated. Ideally, the patient receives sedation prior to pacing, but if the patient is deteriorating rapidly, it may be necessary to start TCP prior to sedation.
For the patient with symptomatic bradycardia with signs of poor perfusion, transcutaneous pacing is the treatment of choice.
Do not delay TCP for the patient with symptomatic bradycardia with signs of poor perfusion. The starting rate for TCP is 60-80/min and adjust up or down based on the patient’s clinical response. The dose for pacing is set at 2mA (milliamperes) above the dose that produces observed capture.
TCP is contraindicated in the patient with hypothermia and is not a recommended treatment for asystole.
Do not use a carotid pulse check for the assessment of circulation as TCP can create muscular movements that may feel like a carotid pulse. Assess circulation using the femoral pulse.
Identification of contributing factors for symptomatic bradycardia should be considered throughout the ACLS protocol since reversing of the cause will likely return the patient to a state of adequate perfusion.
Top Questions Asked on This Page
-
Q: Should I use atropine in all cases of symptomatic bradycardia regardless of the level of block? The prep test for AHA ACLS seems to support giving atropine initially in symptomatic second-degree block type II, but not for complete block.
A: There are a couple of things to mention here. First, atropine may be used for any type of block but may negatively affect outcomes if the bradycardia is being caused by myocardial infarction.
This negative effect may occur because atropine increases the heart rate and myocardial oxygen demand. In the case of bradycardia caused by MI, it would be safer to transcutaneous pace (TCP) at a rate of 60 and move toward some type of cardiac intervention. You should use the 12 lead ECG to help determine MI. This will help determine if atropine may exacerbate the patient’s condition. If the patient has severe symptoms, you should not delay transcutaneous pacing (TCP).
You will usually have time to try atropine as you prepare for TCP.
Second, AHA states “For Mobitz II and complete block (3rd Degree block), atropine should not be relied upon.” This does not mean that it is contraindicated. It just means that it should not be relied upon because there is a good chance that it will not work.
It may not work because atropine blocks the action of the vagus nerve. Atropine works at the SA and AV node through its effect on the vagus nerve, and since conduction abnormalities associated with 2nd-degree block type II and 3rd-degree heart block are below (distal) the site of action for atropine, the drug will typically have an insignificant effect.
-
Q: Why is pacing contraindicated in hypothermia?
A: Bradycardia may be physiologic in the hypothermic patient. This type of bradycardia is an appropriate response to the decreased metabolic rate that normally occurs with hypothermia.
Also the hypothermic ventricle is more prone to fibrillation with any sort of irritation. Thus the irritation of TCP could induce VF. Once the hypothermic ventricle begins to fibrillate, it is more resistant to defibrillation. Warm the patient and then treat any remaining arrhythmias.
-
Q: What is TCP?
A: TCP means transcutaneous pacing.
-
Q: What is chemical pacing?
A: Chemical pacing is when IV medications (epinephrine or dopamine) are used to increase the heart rate rather than the transcutaneous pacing which uses electricity to increase the heart rate.
Khadidja says
I had a case of a medically free pt , post cs. In recovery she developed sinus bradycardia. Hr was between 48/49 when she move it goes up to 60 and down again to 48/45 completely asymptomatic therefore i chosed to monitor rather than giving atropine. After 8h hr dropped tob37 always asymptomatic. 1mg of atropine was given and her hr raised to 107 with high bp and headache. Every thing went back to normal she remained bradycardic 35/38 asymptomatic no atropine giver. 48h laiter her hr went back to normal gradually. Can you coment the case. What could have caused the brady? Was it wise not to give atropine at first? Is it true that asymptomatic brady 37 can cause sudden arrest? Are pst cs pt more exposed to benign brady?
Can you please
ACLS says
Hi Khadidja,
This case of asymptomatic bradycardia post-cesarean section (CS) reflects a pattern that is documented but not very common, and your conservative management was consistent with current recommendations except in the setting of symptoms or hemodynamic instability[1][2][3].
Causes of Bradycardia after Cesarean Section
– Postpartum bradycardia has been linked to increased vagal tone as the body readjusts after pregnancy, the influence of anesthesia (especially spinal or epidural), medication effects (e.g., oxytocics, ergot alkaloids), underlying conduction abnormalities, electrolyte disturbances, and preeclampsia[1][4][5][6][7][8].
– In many documented cases, including large case series, transient hypervagotonic sinus node dysfunction (excessive vagal influence) is suspected, often in entirely healthy patients and typically resolves without intervention[1][9][8].
– Bradycardia is also relatively more common after anesthesia for CS, but is usually benign and self-limited, especially in the absence of hemodynamic compromise or symptoms[5][7][10].
Atropine Use: Was Withholding Initially Appropriate?
– Leading guidelines (e.g., ACLS, StatPearls) specify that atropine is indicated for symptomatic bradycardia—manifested by hypotension, altered mental status, ischemic chest pain, or signs of shock—not for isolated low heart rates without symptoms[3].
– Asymptomatic bradycardia, even down to the 30s, can be observed in certain populations (particularly postpartum, athletes, or after spinal anesthesia) so long as the patient remains stable and well-perfused[1][2].
– Administering atropine in an asymptomatic patient can cause unwanted side effects, including tachycardia, hypertension, and sometimes headache, as occurred in your patient[3].
Risk of Sudden Arrest in Asymptomatic Bradycardia of 37 bpm
– Major studies show that asymptomatic sinus bradycardia—even at rates approaching 30 bpm—rarely results in sudden arrest unless there are underlying conduction abnormalities, structural heart disease, or concurrent conditions affecting perfusion[2][11].
– Routine treatment with atropine is not indicated if there are no symptoms; the course is usually benign, but secondary causes (electrolytes, thyroid dysfunction, medications) should be ruled out[2].
– Extremely rare cases of sudden arrest in completely stable, asymptomatic individuals have been described, but these often involve other comorbidities or unrecognized cardiac disease.
Are Post-CS Patients More Exposed to Benign Bradycardia?
– Incidence of benign (usually transient) bradycardia is higher following CS, especially with regional anesthesia, and is frequently linked to a hypervagotonic state or drug effects[5][6][7][10].
– Most such episodes resolve over hours to a few days, as seen in your patient. Only persistent, symptomatic, or hemodynamically significant bradycardia warrants aggressive intervention[1][4][5].
In summary, the approach of monitoring an asymptomatic post-CS patient with bradycardia was consistent with evidence-based practice; atropine is indicated only if bradycardia becomes symptomatic or there is hemodynamic compromise. The risk of sudden arrest from asymptomatic bradycardia at 37 bpm is exceedingly low in otherwise healthy individuals. Post-CS patients, particularly those who received regional anesthesia, are at a somewhat higher risk for benign, self-limiting bradycardia[1][2][3][5].
Sources
[1] Asymptomatic Postpartum Bradycardia: A Case of Spontaneous … https://pmc.ncbi.nlm.nih.gov/articles/PMC12035969/
[2] Evaluation and Management of Asymptomatic Bradyarrhythmias https://pmc.ncbi.nlm.nih.gov/articles/PMC8142361/
[3] Atropine – StatPearls – NCBI Bookshelf https://www.ncbi.nlm.nih.gov/books/NBK470551/
[4] Post-partum maternal bradycardia: A case series and literature review https://pmc.ncbi.nlm.nih.gov/articles/PMC11110741/
[5] Post-partum maternal bradycardia – Sage Journals https://journals.sagepub.com/doi/pdf/10.1177/1753495X231178407
[6] [PDF] Postpartum Maternal Bradycardia Overview http://www.library.wmuh.nhs.uk/wp/library/wp-content/uploads/sites/2/2017/01/Maternal-Bradycardia.pdf
[7] An Observational Study on Arrhythmia During Cesarean Section … https://www.cureus.com/articles/65316-an-observational-study-on-arrhythmia-during-cesarean-section-under-spinal-anesthesia-incidence-risk-factors-and-effects-on-immediate-post-delivery-neonatal-outcome
[8] Postpartum Transient Hypervagotonic Sinus Node Dysfunction … https://www.cureus.com/articles/36687-postpartum-transient-hypervagotonic-sinus-node-dysfunction-leading-to-sinus-bradycardia-a-case-report
[9] [PDF] Transient Sinus Node Dysfunction in a Postpartum Female with … https://scholarworks.utrgv.edu/cgi/viewcontent.cgi?article=1493&context=somrs
[10] Arrhythmias following spinal anesthesia for cesarean delivery https://pmc.ncbi.nlm.nih.gov/articles/PMC3214565/
[11] Sinus Bradycardia – StatPearls – NCBI Bookshelf https://www.ncbi.nlm.nih.gov/books/NBK493201/
My response was aggregated with the help of perplexity
Kind Regards,
Jeff
https://acls-algorithms.com/member-login/
marc david simmons says
I cannot find anywhere why atropine was increased to 1mg from .5mg. Is it detrimental to give .5 mg? I have been giving .5 since 2005. I have never had an issue and do not see why I should change this practice.
ACLS says
The increase in the recommended atropine dose from 0.5 mg to 1 mg in the 2020 ACLS guidelines was based on updated evidence and expert consensus.
The key points for the changes were:
Efficacy: The 1 mg dose is believed to be more consistently effective in treating symptomatic bradycardia.
Safety: The 1 mg dose is still considered safe for most patients. The maximum total dose remains 3 mg.
Simplification: Using a standard 1 mg dose simplifies the protocol and reduces potential dosing errors.
Avoiding paradoxical effects: Very low doses of atropine (less than 0.5 mg) can potentially cause paradoxical bradycardia. The 1 mg dose helps ensure this is avoided.
Not detrimental: Giving 0.5 mg is not considered detrimental or harmful. It may still be effective in many cases.
Clinical judgment: While guidelines recommend 1 mg, clinicians can still use their judgment based on individual patient factors.
If the 0.5 mg dose has been effective in your experience, it’s understandable to be hesitant about changing. It may be worth discussing with your colleagues and institution about adopting the new recommendation. Remember that guidelines are meant to inform clinical practice, but individual patient factors and clinician judgment always play a crucial role in decision-making.
Kind regards,
Jeff
Ryan says
Hello, should i given 3mg (max dosage) of atropine before begin dopamine therapy? Thank you
ACLS says
It is not necessary to give the full 3 mg maximum amount of atropine before moving on to a dopamine or epinephrine drip.
Kind regards, Jeff
MM says
If a patient is unstable and has known third-degree heart block, is atropine still given first-line or is isoprenaline given as this is more effective in such situations?
Thank you :))
ACLS says
The American heart association gives no guidance with regard to the use of isoprenaline.
The following quote is from the American Heart Association Circulation Journal. “Avoid relying on atropine in type II second-degree or third-degree AV block with a new wide-QRS complex. These patients require immediate pacing.”
It also states, “atropine administration should not delay implementation of external pacing for patients with poor perfusion.”
Kind regards,
Jeff
Mustafa says
Hi Jiff
When will say patient with bradycardia is symptomatic ( unstable) , if he has one symptom or more than two symptoms….??
As I know unstable of bradycardia with symptoms ( hypotension, altered mental status, chest discomfort , sign of shock, acute heart failure) ..
Thx u
ACLS says
A patient can be symptomatic without being unstable. Any one of the symptoms that you listed would indicate that the patient is (unstable hypotension, altered mental status, chest discomfort, signs of shock, acute heart failure.)
Kind regards,
Jeff
Barb Dauerty says
Thanks for verifying…