 Tachycardia/tachyarrhythmia is defined as a rhythm with a heart rate greater than 100 bpm.
Tachycardia/tachyarrhythmia is defined as a rhythm with a heart rate greater than 100 bpm.
An unstable tachycardia exists when cardiac output is reduced to the point of causing serious signs and symptoms.
Serious signs and symptoms commonly seen with unstable tachycardia are: chest pain, signs of shock, SOA (short of air), altered mental status, weakness, fatigue, and syncope.
One important question you may want to ask is: “Are the symptoms being caused by the tachycardia?” If the symptoms are being caused by the tachycardia treat the tachycardia.
Causes
There are many causes of both stable and unstable tachycardia and appropriate treatment within the ACLS framework requires identification of causative factors. Before initiating invasive interventions, reversible causes should be identified and treated.
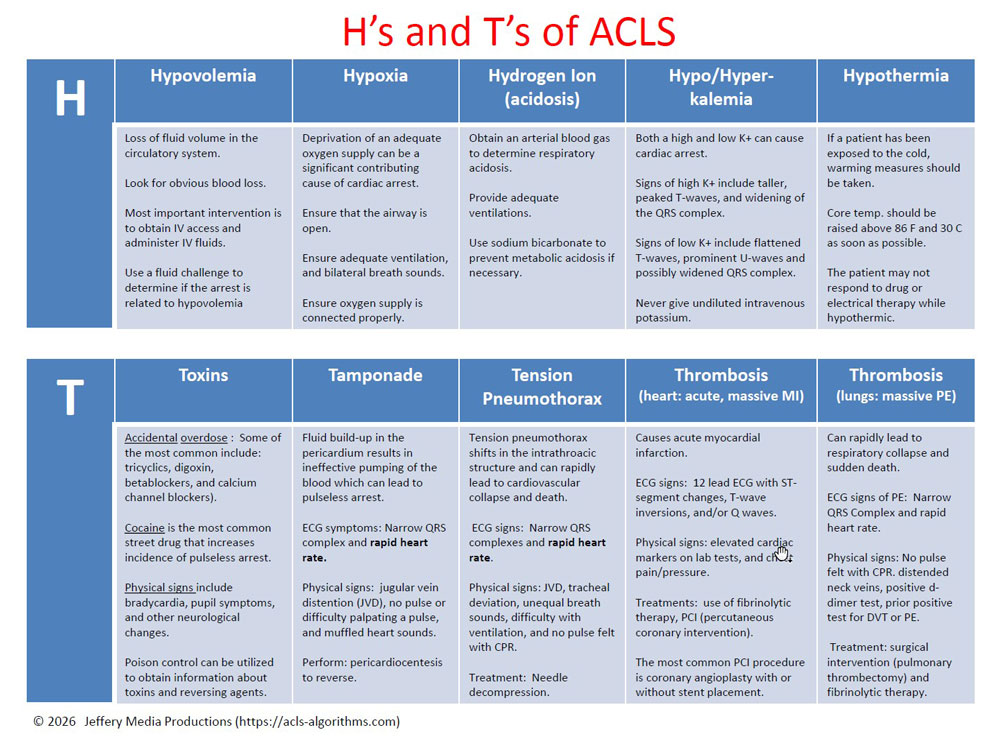
The most common causes of tachycardia that should be treated outside of the ACLS tachycardia algorithm are dehydration, hypoxia, fever, and sepsis. There may be other contributing causes and a review of the H’s and T’s of ACLS should take place as needed.
Click below to view the H and T’s table. When done click again to close the diagram.
H’s and T’s Table
Administration of OXYGEN and NORMAL SALINE are of primary importance for the treatment of causative factors of sinus tachycardia and should be considered prior to ACLS intervention.
Once these causative factors have been ruled out or treated, invasive treatment using the ACLS tachycardia algorithm should be implemented.
Associated Rhythms
There are several rhythms that are frequently associated with stable and unstable tachycardia these rhythms include:
- Supraventricular tachycardia (SVT)
- Atrial fibrillation
- Atrial flutter
- Monomorphic VT
- Polymorphic VT
- Wide-complex tachycardia of uncertain type
ACLS Treatment for Tachycardia
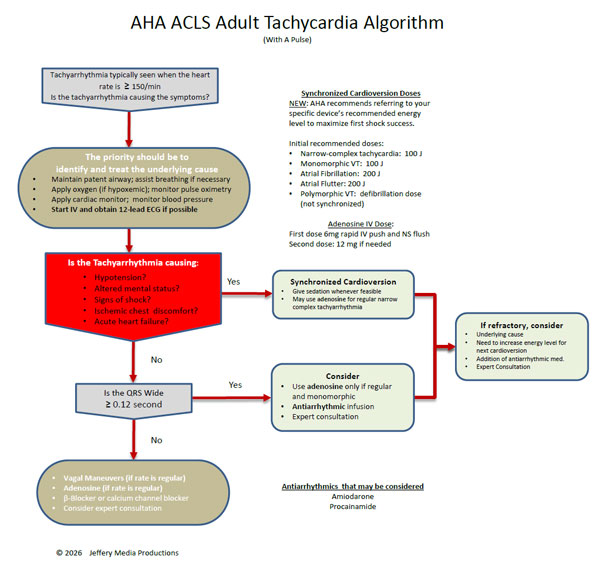
Click below to view the tachycardia algorithm diagram. When done click again to close the diagram.
Tachycardia Diagram
or Members Download the Hi-Resolution PDF Here(This will open in another window.)
The first question that should be asked when initiating the ACLS tachycardia algorithm is: “Is the patient stable or unstable?” The answer to this question will determine which path of the tachycardia algorithm is executed.
Unstable Tachycardia
Patients with unstable tachycardia should be treated immediately with synchronized cardioversion. If a pulseless tachycardia is present patients should be treated using the cardiac arrest algorithm.
The AHA no longer provides specific shock dose recommendations for synchronized cardioversion. Instead, they instruct to refer to your specific device’s recommended energy level to maximize first shock success.
For the purposes of a basic understanding of cardioversion, the information about general shock dosages and recommendations will remain in the content on this website.
The initial recommended synchronized cardioversion voltage doses are as follows:
- narrow regular: 50-100 J; i.e., SVT and atrial flutter
- Narrow irregular: 120-200 J biphasic or 200 J monophasic; i.e., atrial fibrillation
- Wide regular: 100 J; i.e., monomorphic VT
- Wide irregular: defibrillation dose (not synchronized)
Stable Tachycardia
Patients with stable tachycardia are treated based upon whether they have a narrow or wide QRS complex. The following flow diagram shows the treatment regimen for stable tachycardia with narrow and wide QRS complex.
- Stable (narrow QRS complex) → vagal maneuvers → adenosine (if regular) → beta-blocker/calcium channel blocker → get an expert
- Stable (wide/regular/monomorphic) → adenosine → consider antiarrhythmic infusion → get an expert
Mustafa says
Hi
my question
1- How long will press bottom ( Pad ) when perform cardioversion ..??
2- when administered amidrone 150 mg over 10 mit ( 1 amp = 150 mg ) how will dilute it and which by saline or Dextrose .??
ACLS says
1. I do not understand your first question. I do not understand what you mean when you say “how long will press bottom?”
2. Amiodarone is diluted with D5W. 150ml of amiodarone in 100 ml of D5W.
Kind regards,
Jeff
Richard Kerio says
if we have a patient with old AFib and end stage ckd presents with a pulmonary edema..is it recommended to do an electric sync schock?? and why??
ACLS says
There are a number of variables within your scenario. If the patient is stable this scenario would require prior consultation with a cardiologist and a nephrologist prior to any intervention.
If the patient is unstable and the instability is clearly related to the atrial fibrillation then a cardioversion may be necessary. Other causes would need to be ruled out prior to any emergency intervention. There are other interventions that can be performed for chronic or new onset atrial fibrillation with a rapid ventricular rate.
This scenario is definitely beyond the scope of basic advanced cardiovascular life support and there would not be a clear-cut answer.
Kind regards,
Jeff
SUDHIR DEY says
Dear Sir : I completed my ACLS. But your site for cardiology is excellent . I want to practice it through out the year. I want more megacode series and case history. How to get it. In tachycardia,pt is stable ,pulse palpable but monitor shows HR 110 to 140 ,varying time to time. At this stage is it justified to use adenosine? I will renew my membership. pl reduce the cost if possible. Thanks.
Dr. Dey.
ACLS says
Adenosine would not be justified in this situation. A sustained heart rate of 110 to 140 would not be considered SVT. A 12-lead ECG would also need to be obtained. Other causes of the tachycardia should be ruled out, and as long as the patient is stable they should be evaluated by a cardiologist.
Typically, SVT will have a rate much higher than 110-140 per minute.
Kind regards,
Jeff
Sheeraad says
SVT has no p wave. Do the ecg to make sure
Norma Chesney says
I know no questions are stupid, but I have a hard time with “synchronized cardioversion, and unsynchronized”. Could you explain this in simple terms?
Thanks…by the way…love your site!!
Jeff with admin. says
This webpage provides a simple explanation: synchronized vs unsynchronized cardioversion
Kind regards,
Jeff
Anthony Price says
Let’s say an unstable A-fib patient was cardioverted at 50 J, then 100 J. If he/she still did not convert, should I continue cardioverting and higher and higher joules?
Jeff with admin. says
I have had this discussion with several cardiologists and they tell me that if the lowest dose fails then they go straight to the maximum dose that the machine will deliver. They say that this gives them the best results.
AHA does not have a specific recommendation, and I think the above recommendation is good.
Kind regards,
Jeff
Enrique Luis Nuguid says
Hi
Just to clarify the initial dose of shocking, does This mean we can increase the initial dose if the rhythm is not converted?
Jeff with admin. says
Yes, that is correct. You can increase shock doses when using synchronize cardioversion for unstable tachycardia.
Kind regards,
Jeff
Enrique Luis Nuguid says
So if my patient with unstable svt did not convert with 100j I can move up to higher dose?
Jeff with admin. says
Yes, you should increase the shock does if 100 J does not convert unstable SVT.
Kind regards,
Jeff
lawal2022 says
Hi Jeff
Thanks for an amazing website.
How long should you do vagal maneuvers whilst preparing Adenosine?
Regards and thanks
Alice
Jeff with admin. says
Two or three attempts with vagal maneuver’s should be sufficient. This should not take longer than 5-10 minutes. If conversion has not occurred after the third attempt with vagal maneuver’s then it’s unlikely that it will work.
You have to realize that these patients are stable. The timeframe is not as critical. Once you have established that vagal maneuvers are not likely to succeed then move on to adenosine.
Kind regards,
Jeff
kran says
best way to use a the vagal maneuver is combining carotid massage with valsalva maneuver. That gives you a very high conversion rate, its amazing to see how a patient not responding to carotid massage , suddenly responds to addition on valsalva.
thank you for your amazing effort on this site
regards
Hosh26 says
What about torsades de poites, is it a shockable rhythm?
Jeff with admin. says
It depends upon the patient’s condition. It is a shockable rhythm. It’s very unlikely that synchronized cardioversion will be possible because of the variation in the QRS complexes. If the patient is unstable or pulseless with torsades then defibrillation is indicated.
In the unlikely chance that the patient is in torsades and is stable then antiarrhythmics and or magnesium can be used. Preparation for defibrillation should be made because this rhythm can quickly become unstable.
Kind regards,
Jeff
Abe says
I’ve read conflicting recommendations about treatment of unstable (impaired perfusion but with a pulse) polymorphic VT / torsades. Polymorphic VT is a subset of irregular VT. Are there situations in which the treatment of polymorphic VT differs from other irregular VT?
If not, the recommendations above are clear enough- defibrillation not synchronized cardioversion. Are there any situations in which synchronized cardioversion is used for irregular VT?
Thanks!
Jeff with admin. says
Defibrillation is recommended for all polymorphic ventricular tachycardia. The reason for this is that the defibrillator will not synchronize with the irregular rhythm and therefore shock delivery will not be able to occur.
Defibrillation allows the defibrillator operator to manually provide shock and therefore bypasses synchronization.
Kind regards,
Jeff
Mackenzie Corrigan says
Hello,
What is the specific dosing for the antiarrthymthic infusion for the following tachy situation : (wide/regular/monomorphic) → adenosine → consider antiarrhythmic infusion → get an expert consultation
Also, is only one dose of Adenosine (6 mg IV rapid infusion) considered the correct dosing for the first line of treatment of this tachy?
Thank you!
This site is extremely helpful!
Jeff with admin. says
The dosing for adenosine would be 6 mg and if 6 mg fails then attempt 12 mg.
If the adenosine fails to convert the rhythm then you would use amiodarone and this is the infusion information:
Amiodarone 150 mg over 10 minutes → repeat as needed if VT recurs → maintenance infusion of 1mg/min for 6 hours
This information can be found on page 133 three the AHA ACLS provider manual.
Kind regards,
Jeff
Seth says
I thought adenosine was only used for narrow complex tachyarrhythmias?
Jeff with admin. says
This is the AHA statement regarding the use of adenosine with wide complex tachycardia.
Reference
Kind regards, Jeff
Rick John says
Hello, if the patient with very rapid VT (200bpm) with unstable hemodynamic, altered mental status and rapidly deteriorate to LOC, and pulse is not palpable alternated with sometime very very weak pulse, his documented LV function is very altered (LVEF 10%). Should we give immediately defibrillation or cardioversion? What this patient considered to be in pulseless VT?
Thanks
Jeff with admin. says
You could attempt synchronized cardioversion. There is a good chance that the machine can sync with the patient’s rhythm and synchronized cardioversion can be performed. If the synchronization fails then you can move to defibrillation.
Pulseless would be would there is not palpable pulse at all. This case would not be considered pulseless.
Kind regards,
Jeff
Theresa Broetzmann says
Jeff,
Thank you so much for your services and this site! I will use this site for all future ACLS and PALS renewals. I was so impressed with this site that I have shown it to numerous colleagues and our educator for new hires and people needing renewals. Have a great day!
Jeff with admin. says
Thanks so much for your encouraging words. I really appreciate it. Thanks also for passing the site along to others.
Kind regards,
Jeff
See Thao says
I know this is maybe a dumb question but can you tell me what does Regular and Irregular mean in the EKG waveform?
Jeff with admin. says
Regular means that the R to R interval is the same throughout the EKG tracing. Each QRS complex falls equidistantly every time.
Irregular means that the R to R interval is different throughout the EKG tracing. There is variability between when the QRS complexes fall.
Kind regards,
Jeff
Nickie says
Hi
I was wondering why is it necessary to shock aftereach medication is given
Thank you
Jeff with admin. says
I’m assuming that you are referring to the left branch of the cardiac arrest algorithm.
A shock is given after each round of CPR if the rhythm remains VF or pulseless VT.
The administration of medications has nothing to do with when shocks are given.
The only requirement with regard to the administration of medications is that they be given while chest compressions are being performed.
Kind regards,
Jeff
sheikh tariq says
HELLO,IF PATIENT IS UNSTABLE WITH SINU TACHYCARDIA HR >150/MIN IS CARDIO VERSION INDICATED IN THAT CASE.ANY REFRENCE FOR THAT.IN SINUS TACHY PRIORITY IS TO TREAT UNDERLYING CAUSE,AM I CORRECT OR NOT. THANKS N REGARDS
Jeff with admin. says
If you are dealing with Sinus Tachycardia, it is very unlikely that you will see rates greater than 150. Rates greater than 150 with sinus tachycardia do happen and this is where caution is recommended.
If you are for sure that you are dealing with sinus tachycardia, you would want to find and treat the underlying cause of the increased heart rate. If no underlying cause can be found your probably not dealing with sinus tachycardia and can proceed with synchronized cardioversion or adenosine.
True sinus tachycardia will not respond to cardioversion and is contraindicated.
AHA ACLS Provider Manual pg. 140
“Sinus tachycardia is caused by external influences on the heart, such as fever, anemia, hypotension, blood loss, or exercise. These are systemic conditions, not cardiac conditions. Sinus tachycardia is a regular rhythm, although the rate may be slowed by vagal maneuvers. cardioversion is contraindicated.”
Kind regards,
Jeff
Nickicia Campbell says
Hi Jeff,
Thanks so much for this site. I have learnt alot so far. Regarding the question, I have been taught the same info regarding sinus tachy as u mentioned, but also that Atrial Flutter with 2:1 block, can look like Sinus tachy with an exact rate of 150 bpm, on an ECG….Sometimes slowing the rate on the ECG machine can reveal this rhythm. And if unstable atrial flutter then treat accordingly, if not then look for other causes of instability? I would appreciate your response to this
Jeff with admin. says
Your statement above would be appropriate for the situation as long as the atrial flutter was causing an unstable state in a patient.
Adenosine maybe used to slow the ventricular rate in order to see any underlying atrial arrhythmias.
Synchronized cardioversion would be recommended for unstable atrial flutter. However, a transesophageal echocardiogram should be performed prior to treating new onset atrial flutter when the time of onset is not known. This echocardiogram is for ruling out thrombus. There is a potential for thrombus development and thrombus must be ruled out prior to cardioversion.
If a patient is stable and has new onset atrial flutter, consultation with a cardiologist would be recommended prior to any treatment.
Kind regards,
Jeff