Ventricular fibrillation (VF) occurs when there are uncoordinated contractions within the ventricles of the heart. The primary cause of VF is hypoxia (lack of oxygen) to the heart muscle, which causes hyperirritability in the cardiac muscle tissue.
As a result, multiple muscle cells within the ventricles simultaneously fire as pacemakers causing a quivering or fibrillation that is ineffective for adequate cardiac output.
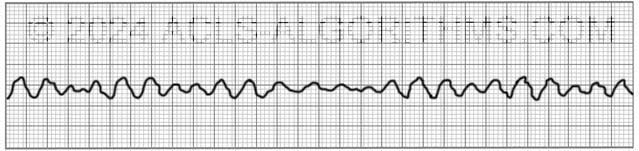
The two images show what ventricular fibrillation will look like on an EKG rhythm strip.
VF can rapidly lead to heart muscle ischemia, and there is a high likelihood that it will deteriorate into asystole.
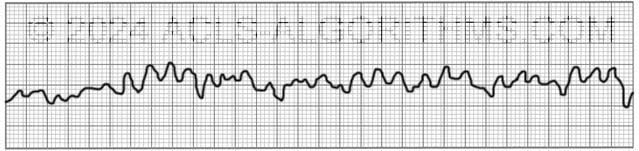
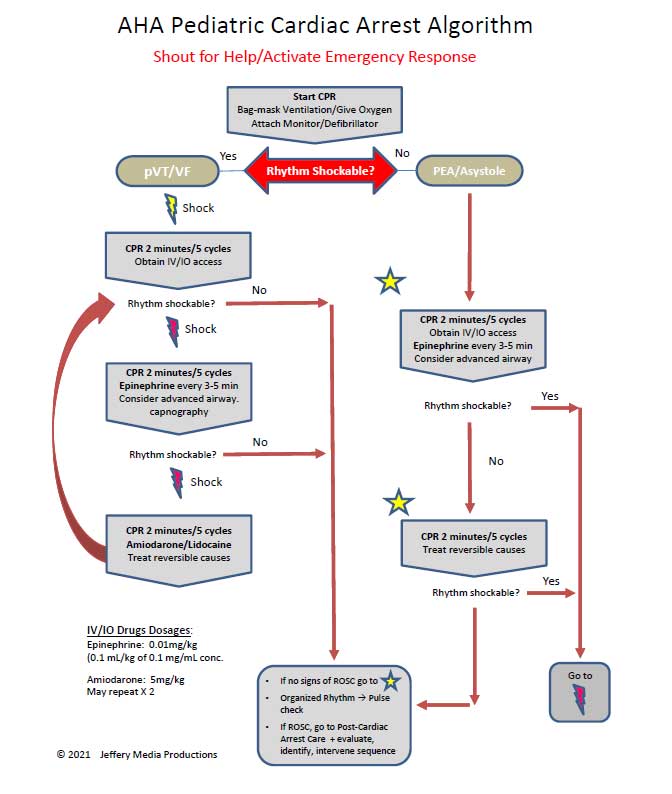
Ventricular fibrillation is treated using the left branch of the cardiac arrest algorithm. Click below to view the cardiac arrest algorithm diagram. When done click again to close the diagram.
Cardiac Arrest Diagram
Click to view, and click again to close the diagram.
PALS Cardiac Arrest Diagram
Ventricular fibrillation is always pulseless and must be confirmed by EKG or defibrillator monitor. Defibrillation is the treatment of choice and should occur as soon as possible.
The video below shows an example of what ventricular fibrillation will look like when you see it on the defibrillator monitor. Please allow several seconds for the video to load. (7.24mb)
Click for next Rhythm Review: Pulseless Electrical Activity
Top Questions Asked on This Page
-
Q: Why does it say VFib is always pulseless? My thinking is an organized rhythm with no pulse will be PEA, then should be treated as on R branch of the cardiac arrest algorithm.
A: Ventricular fibrillation is not an organized rhythm. It is a chaotic and disorganized rhythm. There is no organization to the rhythm. There are no p-waves and no QRS complexes.
-
Q: Which concentration of Lidocaine is given intravenously in ACLS considering that there is the local anesthetic as well. Is the 2% safe?
A: Typically, lidocaine for IV infusion is mixed 2000 mg lidocaine in 500 ml. This works out to a 4 mg/ml dilution.
Two percent lidocaine is a 20 mg/ml. This 20 mg/ml would need to be diluted to obtain the 4 mg/ml dilution.
You would not want to give 2% lidocaine without diluting to 4 mg/ml. The main reason for dilution is to avoid rapid high plasma concentrations and reduce toxicity risk -
Q: When does the sodium bicarb injection need to be administered and when does the lidocaine IV need to be administered?
A: Here is the AHA position on Sodium Bicarbonate:
“In some special resuscitation situations, such as preexisting metabolic acidosis, hyperkalemia, or tricyclic antidepressant overdose, bicarbonate can be beneficial (see Part 10: Special Circumstances of Resuscitation).
However, routine use of sodium bicarbonate is not recommended for patients in cardiac arrest.”
Here is the AHA position for Lidocaine:
“There is inadequate evidence to support the routine use of lidocaine after cardiac arrest. However, the initiation or continuation of lidocaine may be considered immediately after ROSC from cardiac arrest due to VF/pVT.
Lidocaine may be considered as an alternative to amiodarone for VF/pVT that is unresponsive to CPR, defibrillation, and vasopressor therapy.
runtherace10 says
Just signed up and having a great time studying this. I’m motivated every time I login to learn more! Question about the left branch of the pulseless arrest algorithm. After you get down to the bottom of the flow chart (CPR 2 minutes/5 cycles) and give Amiodarone and treat reversible causes, the arrow goes back up to the top of the first box in the flowchart. I’m assuming that you continue with CPR 2 minutes/5 cycles (obviously IV/IO access has already been obtained so no need to repeat this again). But if the rhythm is shockable and you administer the shock, do you give a second round of Epinephrine every 3-5 minutes again and if you need to perform another shock do you give another round of Amiodarone again (and so on if you have to keep repeating the loop)? Thanks!
Jeff with admin. says
The medications are basically on their own timeline. Amiodarone is usually only given twice 300mg and then 150mg. After this, the patient has been so long in cardiac arrest there is little likelihood that ROSC will be achieved.
Regarding epinephrine, the first dose is given after the second shock during CPR and then it is on it’s on time schedule and given every 3-5 minutes. The physical actions of CPR-Rhythm check-Shock are basically what you are doing for the repeating loop. Hope this makes sense.
Kind regards,
Jeff
IS says
Hi, I wanted to clarify something: you mention that EPI is given after the 2nd shock. If that is the case, when is the first shock administered? Immediately once the defib pads are attached?
SOrry, if it’s a dumb questions, but just getting reacquainted with the subject- it’s been awhile!
thanks!
Jeff with admin. says
It depends on if the cardiac arrest was witness or unwitnessed. If the cardiac arrest was witnessed then you immediately shock the pt. If the cardiac arrest was unwitnessed, you will provide 5 cycles of CPR and then shock.
Kind regards,
Jeff
pinjala madhusudana rao says
today i had one 61 oldman with acute anterolateral MI. his intial bp-76/42. i gave fluid challnge- bp improved to 116/80. given asprin 300mg + clopidogrel 300mg. gtn withheld due hypotension. during observation he developed vf. i gave intial shock-200joules (biphasic). reverted to sinus rhythm. after 5monites he developed vt followed by vf. second shock of 360 joules given. is it correct to give intial 200j then 360 joules?
Jeff with admin. says
You could have given 300 J for the second dose but many MD’s just go straight to 360 J. What you did was appropriate. AHA ACLS guidelines say “200 then 300 then 360,” but these are just recommendations. What you did was OK. A heparin drip should also have been started and he should have received coronary intervention asap.
Kind regards,
Jeff
john walter nayga says
sir good day just want to clarify is it ok to give shock even if the patient is concsious or need to sedate d patient first? thank you sir.
Jeff with admin. says
It is ok to give a shock to a patient that is conscious. It is not preferred, but in an emergency, it can be done. I have seen this done several times.
Also, there are some people who have internal defibrillators that shock them when there heart goes into VT.
It is definitely not a pleasant feeling and light sedation is preferred.
Kind regards,
Jeff
fa1th15604 says
If it is Vfib is pulseless, then why is it shockable? Why wouldn’t we follow right side of algorithm?
Jeff with admin. says
VF and Pulseless VT are treated using the left branch of the pulseless arrest algorithm. Both VF and pulseless VT respond quite well to defibrillation and the left branch of the pulseless arrest algorithm has proven to be the most effective method of treatment for VF.
Kind regards,
Jeff
slayer says
Well why call it “pulseless VF?” Is there such a thing as VF with a pulse?!? When you put “pulseless” in front of VF/VT it confuses students new to ACLS. When new students try to figure this out for the first time seeing “pulsless” then advising a shock is confusing, since Pulseless Electrical Activity dosnt require a shock. Its ok to remind people that VF/VT patients wont have a pulse, but putting “pulseless” in the title will lead to unnecessary confusion between VT/VF and PEA. (I know a little studying will clear this up but I can see how confusing and frustrating this can be for first timers.)
Jeff with admin. says
I’m not sure where you saw pulseless VF. VF is always pulseless. In several places I have written Pulseless VT/VF and this means pulseless VF and VF.
You will use defibrillation on pulseless VT. You will not use defibrillation on VT. VT may have a pulse and in the case that it does, you will use synchronized cardioversion. You have to clarify on whether you are dealing with pulseless VT or VT.
I like to explain it by stating that Pulseless VT and VF are the two exception to the rule when it comes to PEA. This is why there are two branches to the pulseless arrest algorithm. The left branch for Pulseless VT/VF and the right branch for PEA/Asystole.
Thanks for helping to clarify.
Kind regards,
Jeff
KIM says
this site is really helpful..:) i just wanted to ask something.. is it safe to deliver a shock when the patient is hooked with oxygen?
Jeff with admin. says
As long as the oxygen is not blowing directly across the chest, it is on to shock the pt. the risk of arching is quite low of pads are connected properly.
Kind regards,
Jeff
Blonde4fun says
By far the best ACLS tutorials! Lots of great tips on how to distinguish rhythms (especially the heart blocks) and explanations that are simple and easy to remember. Thank you for all the time and energy you put into your work. It makes my job of passing ACLS easier.
Celeste Hovagimian says
I’m new at this. How can you distinguish between pulseless ventricular tachycardia and ventricular fibrillation on an ECG strip?
Jeff with admin. says
Ventricular fibrillation will be very disorganized and will not have a pattern. Also, you will not be able to determine the heart rate because the rhythm is disorganized.
Ventricular tachycardia will have a very rapid rate which usually greater than 180/min. The rhythm will appear organized and you should be able to count the beats, but the rate will be extremely high.
I would encourage you to review the above page and also the link below:
https://acls-algorithms.com/rhythms/pulseless-ventricular-tachycardia
Kind regards,
Jeff
aclsnursewh says
I am a new grad and my first ACLS course is coming up very soon!! I want to pass! So far I love the videos and information available. Thank you
DB_EMT_9999 says
The videos are great… really gets some adrenaline going!
Thomas A. Lucas, M.D. says
My goodness! This is shocking! Please keep up this beautiful, well constructed helpsite. Out here in the boonies we need the help. THANKS!
siobhansiobhan says
lol shocking har har 🙂 i’m enjoying learning with the discussions underneath, and i’m enjoying this too. resident in fam med doing emerg
poonam says
This is site is definitely very helpful and i hope that it remains helpful in future. I love this site, thank you so much.
DR.NOOR MUHAMMAD AHMED says
THIS SITE HELPED ME ALOT IN PASSING MY 1ST ACLS IN 1ST ATTEMPT… THANX AND LOVE TO THIS SITE FROM AL QASSEM SAUDIA ARABIA..
TysonKuch says
So much emphasis is placed on: Epi, Vasopressin and Amiodarone. How do you know when/if to give Lidocaine during Cardiac Arrest?
Thanks!
Jeff with admin. says
The overall benefits of lidocaine for the treatment arrhythmias in cardiac arrest has come under scrutiny. It has been shown to have no short term or long term efficacy in cardiac arrest.
During a code if you have already use the 2 doses of amiodarone and the code continues then you could at this point initiate the use of lidocaine. I have seen lidocaine used only once in a code over the last 5 years.
It does seem to be falling out of use. On the other hand, I have seen amiodarone used effectively several times. When I say effectively, I mean that the patient regained ROSC.
I cannot say what the long term outcome was in these situations.
No medication has been shown to positively benefit survival to hospital discharge according to the AHA, but both epinephrine, vasopressin, and amiodarone have been shown to improve ROSC in cardiac arrest.
Kind regards,
Jeff
Hammod Alshabibi says
Am gonna this month for acls certificate…
And Am very glad to find this website
Trang Nguyen says
I need to have ACLS Reneal next month. I am glad to find this site. It iks very clear, detail, understandable. I will be confident to take my reneal next month. Thanks
chriscyn01 says
thank you so much this has really been a good tool for me to prepare for acls
shola_82 says
i was adivised once that you dont shock for fine v-fib. is this true?
Jeff with admin. says
Fine VF is VF and it should be shocked as with a distinct VF. Kind regards, Jeff
Maryanne c says
Shola with asystole you don’t shock, however, I have read that fine vfib can look like asystole and there is some literature that says you should shock with asystole in case it is really fine vfib