
SVT is a broad term for a number of tachyarrhythmias that originate above the ventricular electrical conduction system (Purkinje fibers).
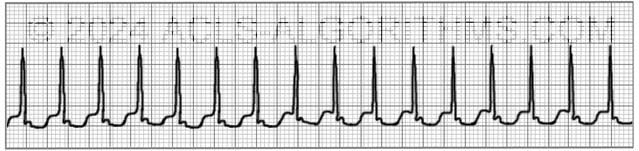
Classic Paroxysmal SVT has a narrow QRS complex & has a very regular rhythm. Inverted P waves are sometimes seen after the QRS complex. These are called retrograde p waves.

The heart fills during diastole, and diastole is normally 2/3 the cardiac cycle. A rapid heart rate will significantly reduce the time which the ventricles have to fill. The reduced filling time results in a smaller amount of blood ejected from the heart during systole. The end result is a drop in cardiac output & hypotension.
With the drop in cardiac output, a patient may experience the following symptoms. These symptoms occur more frequently with a heart rate >150 beats per minute:
- Shortness of air (S)
- Palpitation feeling in chest (S)
- Ongoing chest pain (U)
- Dizziness (S)
- Rapid breathing (S)
- Loss of consciousness (U)
- Numbness of body parts (S)
The pathway of choice for SVT in the tachycardia algorithm is based on whether the patient is stable or unstable. The symptoms listed above that would indicate the patient is unstable are noted with the letter (U). Stable but serious symptoms are indicated with the letter (S).
Unstable patients with SVT and a pulse are always treated with synchronized cardioversion. The appropriate voltage for cardioverting SVT is 50-100 J. This is what AHA recommends and also SVT converts quite readily with 50-100 J.
Below is a short video which will help you quickly identify supraventricular tachycardia on a monitor.
Please allow several seconds for the video to load. (4.37 mb)
Click for next Rhythm Review: Atrial Flutter
Questions Asked On This Page
-
Q: What are vagal maneuvers?
A: A vagal maneuver is a technique by which you attempt to increase intrathoracic pressure which stimulates the vagus nerve. This can result in slowed conduction of electrical impulses through the AV node of the heart. The following methods can be used.- Cough Method: Have a patient cough forcefully. This is a simple form of vagal maneuver. A cough stimulates an increase in intrathoracic pressure which will stimulate the vagus nerve. This can result in slowed conduction of electrical impulses through the AV node of the heart.
- Straw Method: Have the patient blow forcefully through a straw for 3-5 seconds.
- Bear down Method: Have the patient bear down and strain. Kind of like how a person might strain when having a bowel movement.
- Syringe Plunger Method: First, show the patient how easy it is to move the plunger by pulling it back and forth in within the syringe. Now instruct the patient place their mouth over the exit end of the syringe and attempt to blow the plunger out of the syringe. Have them blow for 3-5 seconds.
- Abdominal Pressure Method: Press into the patient’s abdomen while they contract and resist pressing into their abdomen.
- Ice Method: Quote from a healthcare provider: “We had a kid (approximately 12 yrs old) present to our ER in SVT, instead of using drugs and vagal maneuvers we dunked his face in a bucket of ice twice, and it immediately & effectively brought the heart rate down. We observed him for a period of time, and the kid was fine. Worked wonders! Young army doctor’s idea!”
-
Q: I can’t distinguish the sinus tachycardia example from the three re-entry SVT examples on the pre-test no matter how long I stare at the strips…they look identical to me. Help please, and thanks.
A: On the Pretest at the AHA website, Look at each image carefully. Don’t try to over-observe. Just look at each one and notice how many QRS complexes there are.
There are almost double the amount of QRS complexes in all of the SVT when compared to the Sinus Tachycardia. This is the easiest way to tell SVT from Sinus tachycardia. Also, P-waves are only clear in the sinus tachycardia. Most of the time with SVT you will not be able to see the p-waves. SVT rate will usually be greater than 150 and Sinus tachycardia will be less than 150. -
Q: Let me get this straight. Svt is a heart rate greater than 150 with conduction at or above the av node?
A: That is correct.
Dayo says
What’s the difference between a stable and unstable patient. Does dsypnoea and palpitations in a patient discovered to have an SVT make him unstable. Would it be right to shock him immediately or better to do Valhalla manoeuvre then adenosine algorithm.
Jeff with admin. says
The main indication of a patient that is unstable are as follows:
1. Altered mental status
2. SBP less than 90 (hypotension)
3. Signs of shock
4. Ischemic chest discomfort
5. Acute heart failure
The patient with dyspnea and palpitations would not necessarily be unstable, and it would most likely be ok to attempt vagal maneuvers then adenosine prior to any attempt with cardioversion.
Kind regards,
Jeff
ALEJANDRO TERRAZAS says
Sorry the errors!
Kelly says
In the third example on the video it states that you can see p waves. Well, if that’s true, then where are the T waves? In the explanation blurb at the beginning it says that p waves can be buried in the qrs. How are you ever supposed to know if you are looking at p waves or t waves?
Jeff with admin. says
With SVT, It can be difficult to differentiate the p-waves from the t-waves. Most of the time p-waves will not be present due to the rapid HR involved with SVT.
One way to differentiate is to give adenosine to temporarily slow the heart rate. This will give you a better look at the underlying rhythm and help to diagnose the underlying rhythm.
Kind regards,
Jeff
ALEJANDRO TERRAZAS says
Ni jeff. Another forma to find p waves and t waves in some cases justo gain 2 mV and increase TVE speed 50mm/sec. Bye!
Malcolm says
Will synchronised cardioversion always convert an unstable SVT? and if not is it acceptable to administer adenosine in the case of a “SVT refractory to cardioversion”.
Jeff with admin. says
Synchronized cardioversion works over 90% of the time for standard SVTs which are AVRT and AVNRT. Adenosine is not the treatment of choice for unstable SVT.
Kind regards,
Jeff
Tray Ross says
In the case sync cardiovert does not work, try running an epi drip (2-10 mcg/min titrated to effect), or DOPamine drip ( 2-20 mcg/kg/min titrated to effect), per ACLS protocol.
Jeff with admin. says
Epinephrine and dopamine infusions would not be indicated for the treatment of unstable SVT.
Epinephrine and dopamine infusions are used within ACLS protocol for the treatment of bradycardia and hypotension in the post-arrest period.
Kind regards,
Jeff
sheila says
How can you tell the difference between SVT and Atrial Tachycardia? The strip I have has a rate of 180, regular rate, distinguishable P waves. I say SVT but it’s Atrial Tach?
Jeff with admin. says
Atrial tachycardia is a form of SVT. Atrial tachycardia means that the tachycardia originates in the atria but not from the SA node.
When describing a tachycardia that originates in the atria but outside of the sinus note, another term used is supraventricular. Thus, atrial tachycardia is essentially the same thing as SVT.
Kind regards,
Jeff
Todd says
Svt = a rate > 150 bpm
bfemtrn16 says
I would recommend you reading this article.
http://www.ems12lead.com/2013/04/30/the-trouble-with-sinus-tachycardia/
I noticed you stated “SVT = a rate > 150bpm”. I quote “When sinus tachycardia occurs at high rates, our ability to correctly differentiate it from other types of SVT apparently decreases. P waves start to blend into the T waves. Instead of talking about discreet stand alone P waves, we talk about “notches” and “bumps”. It is all too easy to look at a rate >150 and simply call it “SVT”.
rosiemae says
Hi Jeff Great website!!! However, I have returned for my recertification, which is to take place at UCMC in Cincinnati, Ohio. The education department sent me a ACLS study guide. The study guide “ACLS Crucial Management Considerations & Teaching Points” for Superventricular Tachycardia is to try vagal maneuvers. In addition, Adenosine 6mg can be given, repeat 12mg and then another 12mg rapid IV push. I was under the impression that Adenosine can be given just 2 times (6mg, 12mg). Please advise. Thank you. Kim
Jeff with admin. says
Giving a second dose of 12mg of adenosine is fine. This is not clear in the manual and I do think that AHA will clear this up with their next series of guidelines in 2015. The AHA manual has 6 mg given and then 12 mg. For many years is always listed 6-12-12 and then in 2010 it changed to 6-12. Honestly, I have never gotten a clear answer from AHA. I have been told and have seen that at times a 3rd dose of 12 mg may be necessary. It can be given. Kind regards, Jeff
rosiemae says
Hi Jeff Thank you. In addition, you always respond with Honest answers, the Literature/References for best practices, and thank you for the wonderful website. During my first time of becoming certified for ACLS, I was terrified. However, I came across this wonderful web site (Lucky me), and passed on my first attempt :). Now that recertification is to occur, I feel 100% confident. May God continue to shower blessings on you and your brother. Kim
Jeff with admin. says
Thanks Kim!
marie says
hi
is supraventrical svt the same as paroxymal svt. if not the same please explain the difference
thank you
Jeff with admin. says
Hi ,
Thanks for the question. You asked:
“is supraventrical svt the same as paroxymal svt. if not the same please explain the difference”
SVT is a general term for a number of different arrhythmias that have their origin in the atria hence the name SUPRAventricular.
Paroxysmal SVT is the most common SVT. A person experiencing this type of PSVT may feel the heart rate accelerate from 60 to 200 beats per minute or more. Typically, when it reverts to normal rhythm, this is also sudden. This type of SVT can come and go without any apparent cause.
Kind regards,
Jeff
Mark says
My Question
How I can identify the SVT wide QRS related to antidromic re-entry and stable patient with monomorphic ventricle tachycardia in ECG
Jeff with admin. says
This can be very difficult. Differentiation of VT from SVT with aberrancy is not always possible. This web page goes much more into detail on the subject.
Kind regards,
Jeff
NONNIE says
My only complaint about this scenario is the rates of SINUS TACH , SVT are not shown… An experienced nurse can tell just by looking at the monitor … but a newer nurse or student may not especially if this is her/ his first exposure to the information / ACLS. I think rates would be helpful to be posted with changes in rthym.
steve says
SVT normally has a rate of 150 to 250, ST 100 to 150. You should be able to distinguish p waves with ST. Hope this helps
Ted says
Having some difficulty distinguishing SVT, (unless it’s reentry), and sinus tachy. Any helpful suggestions? Thanks!
Jeff with admin. says
The easiest way to differentiate between SVT and Sinus Tachycardia is to simply look at the rate. The rate of sinus tachycardia for a person at rest, in most circumstances, will not exceed 150 bpm. If the rate is high and you do not suspect SVT then you should ask yourself why the rate is high. When a person has SR and an elevated rate, there is a specific reason that is causing the elevated heart rate. (fever, blood loss, dehydration, infection, etc.)
Also the rate of SVT will usually be greater than 150 bpm.
The vague area will be when a person has a rate that is 150-170 bpm.
I hope this helps.
Kind regards,
Jeff
dlambert says
Having trouble understanding if stable or unstable if pt. Is unstable do you go straight to cardioversion. And if so when do you give adenosine.
Jeff with admin. says
Yes, if the pt. is unstable, you go straight to cardioversion. In general, if the patient is stable with narrow complex SVT, you could attempt vagal maneuvers and then adenosine if vagal maneuvers fail.
Kind regards,
Jeff
Melody says
Great resource.
gunnewick-murphy@prodigy.net says
Hi Jeff,
Today I took the pre assessment on the AHA student site and the rhythm section had several reentry tachycardias—what is the difference from other tachycardias and what do I look for on the rhythm strip. I have minimal EKG knowledge and am struggling a bit.
Jeff with admin. says
The most common re-entry tachycardia is SVT. The major difference is the rate will usually be greater than 150/min (often greater than 170) and there will be no p-waves present. The pathophysiology of re-entry tachycardia is a bit complicated to explain without some visuals. Here is a video and another web page about the subject.
http://lifeinthefastlane.com/ecg-library/svt/
https://www.youtube.com/watch?v=PtM58hjSkIw
Kind regards,
Jeff
Rywi says
How can you tell the difference between rapid A-Fib and PSVT when the rate is so high? Both can be treated very differently.
Thanks, Love this site!
Jeff with admin. says
This can be a difficult thing. I have see adenosine as a diagnostic tool to differentiate between the two and it works well.
When you give adenosine, it slows the heart and allows you to see the underlying rhythm. When adenosine is given and the rate temporarily slows, you will see the difference. If atrial fibrillation is present, you will see an irregular rhythm with no p-waves. If the rhythm is SVT, you should see a regular rhythm when the rate is slowed.
Kind regards,
Jeff
Dolly says
If you were performing cardioversion on an SVT rhythm at 200J and then the monitor showed V-tach with no pulse—would you immediately defib at 300 J or into CPR for 2 minutes? If another shock is given that would be two in a row—is that OK to do according to AHA?
Jeff with admin. says
Since the patient had a pulse when in SVT and the change to pulseless VT was witnessed, you would move straight to a shock with 300 J.
Shocking would not be considered two in a row since you had a change in the rhythm. When there is a change in the rhythm, you should start at the top of the algorithm. Also you would be changing form synchronized cardioversion to unsynchronized defibrillation.
Kind regards, Jeff
Ramki. says
300 J Is it monophasic or biphasic ?
.
Big THANKS to JEFF for answering all our questions with such a patience.
Jeff with admin. says
For this website you can assume that any dose that I recommend with by default be biphasic unless otherwise stated. Monophasic is being phased off of the market and biphasic is becoming the standard of care.
Kind regards,
Jeff
ruthblj says
Great site, Just needed information to meet the objectives of ACLS.
I am enjoying it greatly. Thanks a ton for preparing this educational material. It shows great commitment too.