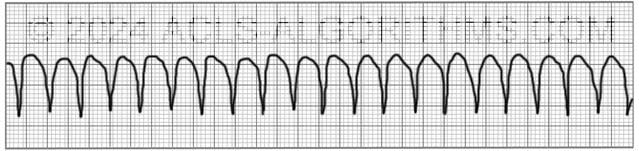
The pulseless ventricular tachycardia rhythm is primarily identified by several criteria. First, the rate is usually greater than 180 beats per minute, and the rhythm generally has a very wide QRS complex.
Second, the patient will be pulseless. And third, the rhythm originates in the ventricles. This is in contrast to other types of tachycardias which have origination above the ventricular tissue (in the atria).
Not all ventricular tachycardias are pulseless, and therefore, pulselessness must be established prior to beginning an algorithm. This is accomplished simply by checking a carotid or femoral pulse.
Pulselessness with a tachyarrhythmia occurs because the ventricles are not effectively moving blood out of the heart and there is, therefore, no cardiac output. Many tachyarrhythmias of a rate >150 will deteriorate into pulselessness if timely treatment is not given.
Pulseless ventricular tachycardia is treated using the left branch of the cardiac arrest algorithm. Click below to view the cardiac arrest algorithm diagram. When finished click again to close the diagram.
Cardiac Arrest Diagram
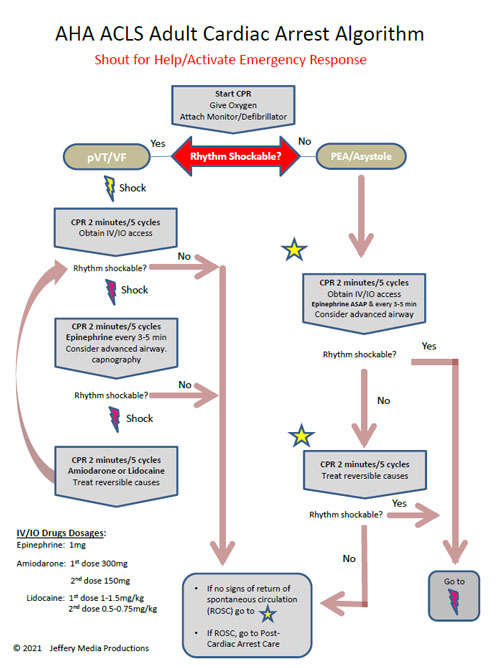
Click to view, and click again to close the diagram.
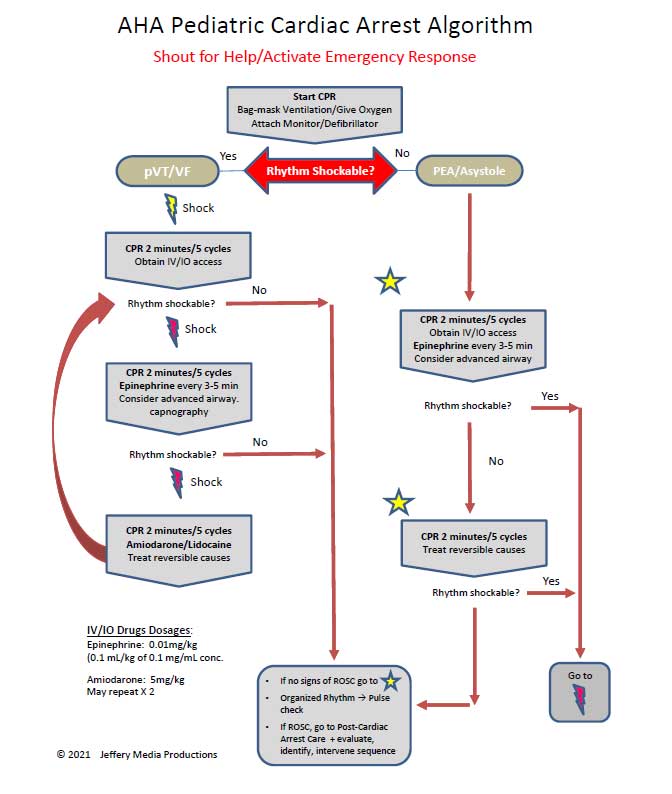
PALS Cardiac Arrest Diagram
Play the video below to see what a Pulseless Ventricular Tachycardia will generally look like on a defibrillator monitor. Allow several seconds for video to load. (4.03 mb)
Click for next Rhythm Review: Ventricular Fibrillation
Top Questions Asked on This Page
-
Q: What happens after the 2nd dose of Amiodarone is given and the patient is still in the same rhythm? Do we give a 3rd dose immediately or rhythm usually changes after 2nd dose?
A: A 3rd and even a 4th dose of 150 mg amiodarone may be administered. The only thing that needs to be taken into consideration is the 2.2-gram maximum dosage for 24 hours. Also, it is unlikely that the rhythm will remain VF or pVT long enough for you to get to the 3rd or 4th dose.
-
Q: What does refractory VT or VF mean?
A: Refractory pVT or VF means that the VF or pVT does not convert to a perfusing rhythm and continues to persist in spite of multiple attempts at conversion with defibrilation, acls drugs, and high quality CPR.
-
Q: After initiating CPR and assessing the rhythm, the patient is in VF/ pVT and the first shock is given, and CPR for 2 mins. Then rhythm check and in VT, should the pulse be checked to confirm pVT?
A: If there is no rhythm change and the same waveform of VT continues, you would not need to perform a pulse check. Performing the pulse check would delay the continuation of chest compressions. Once VT is pulseless it is very unlikely that any VT will be able to produce life-sustaining cardiac contractions.