
The most common cardiac arrhythmia, atrial fibrillation, occurs when the normal electrical impulses that are generated by the SA node are overwhelmed by disorganized electrical impulses in the atria.
These disorganized impulses cause the muscles of the upper chambers of the heart to quiver (fibrillate) and this leads to the conduction of irregular impulses to the ventricles.
For ACLS, atrial fibrillation becomes a problem when the fibrillation produces a rapid heart rate which reduces cardiac output and causes symptoms or an unstable condition.
When atrial fibrillation occurs with a (RVR) rapid ventricular rate (rate > 100 beats/min), this is called a tachyarrhythmia. This tachyarrhythmia may or may not produce symptoms. Significant symptoms that occur are due to a reduction in cardiac output.

The following is a list of the most common symptoms.
- palpitations or chest discomfort
- shortness of air and possibly respiratory distress
- hypotension, light-headedness and possibly loss of consciousness
- peripheral edema, jugular vein distention, and possibly pulmonary edema
For the purpose of ACLS, it is important to be able to recognize atrial fibrillation when the patient is symptomatic. On an ECG monitor, there are two major characteristics that will help you identify atrial fibrillation.
- No p-waves before the QRS on the ECG. This is because there are no coordinated atrial contractions.
- The heart rate will be irregular. Irregular impulses that the ventricles are receiving cause the irregular heart rate.
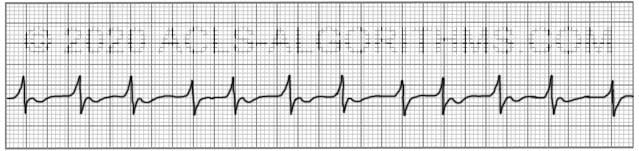
When the heart rate is extremely rapid, it may be difficult to determine if the rate is irregular, and the absence of p-waves will be the best indicator of atrial fibrillation.
ACLS Treatments:
For the purposes of ACLS atrial fibrillation is treated when the arrhythmia/tachyarrhythmia produces hemodynamic instability and serious signs and symptoms.
For the patient with unstable tachycardia due to a tachyarrhythmia, immediate cardioversion is recommended. Drugs are not used to manage unstable tachycardia. The appropriate voltage for cardioverting unstable atrial fibrillation is 120-200 J.
Cardioversion of stable atrial fibrillation should be performed with caution if the arrhythmia is more than 48 hours old and no anticoagulant therapy has been initiated due to the risk of emboli that can cause MI and stroke.
Below is a short video which will help you quickly identify atrial fibrillation on a monitor.
Please allow several seconds for the video to load. (5.11 mb)
Click for next Rhythm Review: Other Tachycardias
Top Questions Asked On This Page
-
Q: To treat a patient with rapid atrial fibrillation (HR >180bpm), can calcium channel blockers be given to help control the rate?
A: Yes, in some cases, calcium channel blockers are a good choice to help control atrial fibrillation with a rapid ventricular rate.
-
Q: What are atrial fibrillation and atrial flutter considered in terms of narrow or wide QRS complexes?
A: Unless there is an underlying block the QRS complex will typically be normal/narrow. There is the possibility of occasional wide QRS complexes due to abnormal ventricular depolarization via an accessory pathway.
-
Q: What does the DC before the word cardioversion stand for?
A: DC cardioversion simply means direct current cardioversion.
paragirl says
What is the recommended cardio version step wise joules for Afib.
ACLS says
AHA Recommends 120 J as the starting dose. 120–200 J is the range that is recommend. It is the physicians discretion for choosing an appropriate dose within the range. Kind regards, Jeff
Sophia says
Can you please discuss the use of AV node blocking agents with Afib and aflutter? How do we treat these stable Afib and aflutter rhythms if we cannot use CCB or BB? for unstable afib and aflutter, we can cardiovert.
ACLS says
Hi Sophia,
Most of your questions are beyond the scope of ACLS.
The use of AV node blocking agents is a common treatment strategy for both atrial fibrillation (AFib) and atrial flutter. These medications, such as beta-blockers or calcium channel blockers (CCBs), can help to slow down the heart rate by blocking the electrical impulses from the atria to the ventricles through the AV node.
However, in some cases, AV node blocking agents may be contraindicated or not well-tolerated by the patient. For example, in patients with severe asthma or certain types of heart block, beta-blockers may not be safe to use. Similarly, in patients with low blood pressure or heart failure, CCBs may not be appropriate.
In these cases, alternative medications may be used to treat stable AFib or atrial flutter. For example, digoxin can be used to control the heart rate in some patients with AFib or atrial flutter. Another option is amiodarone, which is an antiarrhythmic medication that can help to convert AFib or atrial flutter back to a normal sinus rhythm.
If medication is not effective or not well-tolerated, catheter ablation may be considered as a treatment option for stable AFib or atrial flutter. Catheter ablation is a procedure in which a catheter is inserted into the heart to destroy the tissue responsible for the abnormal electrical activity that causes AFib or atrial flutter.
For unstable AFib or atrial flutter, cardioversion may be necessary to restore a normal sinus rhythm. Cardioversion can be performed using either electrical or pharmacologic means.
In summary, the use of AV node blocking agents is a common treatment strategy for stable AFib or atrial flutter, but alternative medications or procedures may be necessary in patients who cannot tolerate these agents. For unstable AFib or atrial flutter, cardioversion may be necessary to restore a normal sinus rhythm.
Kind regards,
Jeff
Barbara Chivers says
Hi We do not have TEE availability in our small hospital. Tertiary care is 90 min away.
Is a D dimer effective in ruling out a clot prior to cardioversion for symptomatic UAF?
We can get those results in 20 min.
Thanks
Barb
ACLS says
A d-dimer can be used to rule out a clot. However, If it’s positive it doesn’t mean they necessarily have a clot.
Kind regards, Jeff
EK says
Hi There
If a patient with Atrial fibrillation suddenly lose pulse, do you follow ACLS protocol which mean this is a PEA, start CPR, Epi… and you do not
Cardiovert
OR do you still consider this unstable and try to cardiovert first?
Jeff with admin. says
If they lose consciousness and there is no palpable pulse then you would treat this as PEA.
If you can not palpate a pulse but the patient remains conscious then you can be assured that they do have a pulse.
In this case, you would want to determine if the patient is unstable. If the patient is unstable with atrial fibrillation then synchronized cardioversion would be the treatment of choice. There are risks involved with providing synchronized cardioversion to a patient with atrial fibrillation if they are not anticoagulated. There is a risk of stroke and it would be wise to rule out thrombus prior to cardioversion if possible. Thrombus can be ruled out with a transesophageal echocardiogram.
Kind regards,
Jeff
Rose says
Can I apply this for nclex RN exam?
Jeff with admin. says
I don’t think that either of the courses offered on this website would be very beneficial for preparing for NCLEX.
The ACLS and PALS courses offered on this website are designed to help people prepare for the American Heart Association ACLS and PALS provider course.
Kind regards,
Jeff
Ashley Heard says
HI Jeff,
I am finding this website to be a great resource. Thank you!
Interpreting ECGs is not part of my job so that is the portion that I am experiencing the most difficulty with. Memorizing and understanding the medications and algorithms is much easier for me.
Can you provide some guidance on how to recognize the difference between atrial and ventricular on an ECG?
Also, how can you know but the ECG alone is the rhythm is pulseless?
Thanks so much for your help!!
Jeff with admin. says
The ventricular portion of the ECG is known as the QRS complex. The QRS complex is the electrical equivalent of the ventricular contraction. If there is no ventricular contraction, there is no pulse. Therefore, if your patient has a pulse, you will see a QRS complex. The QRS complex will be the tallest and most pronounced portion of the ECG reading. The atrial impulses may or may not be present depending on the rhythm. Atrial impulses are recognized on the ECG monitor as P-waves that typically precede the QRS complex. The p-waves are much smaller than the QRS complexes.
A rhythm can be determined to be pulseless simply by manually palpating for a pulse. You cannot determine a pulseless state by only looking at the ECG monitor.
Kind regards,
Jeff
Phil says
Jeff,
What are the rhythms that cardioversion is the first thing that must be done? I mean what shall a beginner like me should see or look that once I see it, it will tell me to perform cardioversion right away? Does it make sense?
Thanks,
Phil
Jeff with admin. says
If you see a patient that is hemodynamically unstable with a wide complex tachycardia, this would be an indication for immediate cardioversion. In fact, any patient that is unstable with a tachyarrhythmia should be prepared for cardioversion. There is a difference between being unstable and symptomatic and knowing that difference is important. Three of the most important signs of instability are changes in the level of consciousness, SBP < 90, and unrelieved chest pain. Kind regards, Jeff
Rachel Jolokai says
Can you further elaborate on difference between symptomatic vs unstable?
Jeff with admin. says
The major difference that will be associated with unstable arrhythmias will be a systolic blood pressure less than 90 mmHg with other signs of poor perfusion.
A patient that is simply symptomatic may have dizziness, tachycardia, weak pulses, etc. but the systole blood pressure remains greater than 90 mmHg, and there are no LOC changes or other signs of poor perfusion.
I hope that makes sense.
Kind regards,
Jeff
LouiseAW says
why the voltage difference in the Cardioversion of Fib Flutter ?
Jeff with admin. says
The reason is that atrial flutter tends to convert with a much lower dose of electricity than atrial fibrillation. Kind regards, Jeff
orangele says
So it is mentioned that blot clots must be ruled out prior to cardioversion for Atrial Fibrillation, but that cardioversion is indicated if the patient is unstable. So therefore I assume that echo is preferred but once patient is unstable that cardioversion must be performed without echo?
Jeff with admin. says
That is correct if a patient has reached the point where there is no other way to keep them stable and cardioversion is indicated then cardioversion may be performed emergently.
I think that this would be a rare occurrence. Usually instability with atrial fibrillation is caused by a rapid heart rate. Typically, you can apply some type of rate control medicaton like cardizem or metoprolol to bring the heart rate down. There are a lot of variables and a lot of options and cardioversion for unstable atrial fibrillation without an TEE would be the last option.
Regards,
Jeff
Nursey54 says
I have to give your course 5 stars! I use it every time I recert for my PACU job and do extremely well.
I plan to do PALS next month. Do you have a course for PALS?
Thanks ! Alice
Monica says
What about this scenario:
82 y/o m pale, cool diaphoretic. No c/o pain and negative on Stroke scale. Pt vs 84/43. 71HR 32R 90%. BGL 63. Pmhx DM HTN MI AFIB CHF HYPERLIPIDEMIA. oral glucose is given and bgl is 224. 12 lead shows AFIB @71 RBBB SUBSEQUENT 12 leads are same with no changes. Rate is between 69 and 102. Cardizem is contra-indicated due to hypotension. No flight is available and closest ER is 1 hour.
Jeff with admin. says
Give an anticoagulant to prevent thrombus. Give Epinephrine or dopamine IV infusion to control hypotension. Transport the patient by EMS to the nearest ICU for evaluation.
Kind regards,
Jeff
Patrick says
Would norepi not be a better choice to avoid the positive chronotropic effect?
Jeff with admin. says
If there were a problem with rate control, you could use norepinephrine. Since the rate is in the 70’s. Dopamine or epinephrine would be acceptable.
There are two other possibilities with this scenario. NSTEMI or sepsis. It would be wise to check a white count. If dopamine is started and the patient develops any chest pain, stop the dopamine and suspect NSTEMI. Norepinephrine would be the best choice if this happens.
Kind regards,
Jeff
Yash says
Since the patient is unstable with SBP below 90. Shouldn’t We perform immediate synchronized cardio version? Correct me if m wrong please
ACLS says
In this situation, the low blood pressure is not being caused by the atrial fibrillation. Typically, atrial fibrillation May cause an unstable scenario when there is a rapid ventricular rate. In this scenario, the rate is controlled. You would need to control blood pressure by utilizing a medication epinephrine or dopamine.
Kind regards, Jeff
abosuyonov says
Thank you .
Just to clarify , even though the ACLS algorithm states that for Unstable Afib we perform synchronized cardioversion, however in reality it appears that for unstable a fib, we stabilize with medications, and once a patient is stable, we cardiovert after doing a TEE. is that correct?
Why don’t we in real life scenario not perform synchronize cardioversion for unstable Afib as it states in ACLS algorithm?
Jeff with admin. says
There is a gray area between stable and unstable with regard to tachycardias like afib and aflutter. If there is no other way of reversing or correcting the unstable condition and cardiac arrest is eminent then synchronized cardioversion is necessary and should be done even if TEE has not been performed.
Kind regards,
Jeff
abosuyonov says
Hello Jeff.
Just to clarify .
For unstable Afib we perform synchronized cardioversion . How can one perform TEE prior to that if pt is symptomatic . It’ll really be almost impossible to do TEE with the symptoms he us experiencing ?
Jeff with admin. says
I personally have never seen a case of unstable afib that needed immediate cardioversion. I have seen some cases of unstable afib that responded well to rate controlling medications, blood pressure infusions, and anticoagulation. After the patient was stabilized with IV medications the TEE is performed and then cardioversion if necessary.
Lets say that a patient is unstable with afib and then has an MI and goes into cardiac arrest (VF). You would take your chances and perform defibrillation. The risks involved in to defibrillating are greater than the risks of thrombus from afib. Hope that makes sense.
Kind regards,
Jeff
Allison says
Gotta say I am taking my recertification tomorrow . I wish I found this sight earlier. Have been looking at it all day. You have really done a great job . Thanks ?